The FEP Prior Auth Form is an essential document for healthcare providers, patients, and insurance companies alike. Its purpose is to facilitate the prior authorization process for medical procedures, ensuring that patients receive the necessary care while adhering to the rules and regulations set by insurance providers. In this article, we will delve into the intricacies of the FEP Prior Auth Form, providing a comprehensive step-by-step guide to help you navigate this complex process.
Understanding the FEP Prior Auth Form

Before we dive into the nitty-gritty of the FEP Prior Auth Form, it's essential to understand its purpose. The form is used to request prior authorization for medical procedures, ensuring that insurance providers cover the costs. This process helps prevent unnecessary procedures, reduces healthcare costs, and ensures that patients receive the most effective treatments.
Benefits of the FEP Prior Auth Form
The FEP Prior Auth Form offers numerous benefits to healthcare providers, patients, and insurance companies. Some of the key advantages include:
• Streamlined prior authorization process • Reduced administrative burden • Improved patient outcomes • Enhanced communication between healthcare providers and insurance companies • Cost-effective care
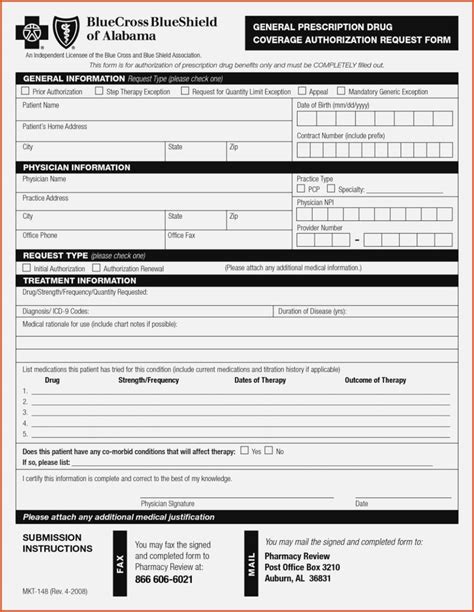
Step-by-Step Guide to Completing the FEP Prior Auth Form

Now that we've covered the basics, let's move on to the step-by-step guide to completing the FEP Prior Auth Form:
Step 1: Gather Required Information
Before starting the form, ensure you have the following information:
• Patient's name and date of birth • Policy number and group number • Procedure code(s) and description • Diagnosis code(s) and description • Requesting physician's name and contact information
Step 2: Complete Section 1 - Patient Information
Fill in the patient's name, date of birth, and contact information.
Step 3: Complete Section 2 - Policy Information
Enter the policy number, group number, and coverage type.
Step 4: Complete Section 3 - Procedure Information
List the procedure code(s), description, and date of service.
Step 5: Complete Section 4 - Diagnosis Information
Enter the diagnosis code(s), description, and relevant clinical information.
Step 6: Complete Section 5 - Requesting Physician Information
Provide the requesting physician's name, contact information, and credentials.
Step 7: Attach Supporting Documentation
Attach any supporting documentation, such as medical records, test results, or physician statements.
Step 8: Review and Submit the Form
Review the form for accuracy and completeness, then submit it to the insurance provider.
Tips for a Smooth Prior Authorization Process
To ensure a smooth prior authorization process, keep the following tips in mind:
• Verify patient eligibility and coverage before submitting the form • Use the correct procedure and diagnosis codes • Provide clear and concise clinical information • Attach all required supporting documentation • Follow up with the insurance provider to ensure timely processing
Common Challenges and Solutions

Despite the benefits of the FEP Prior Auth Form, challenges can arise during the prior authorization process. Here are some common issues and solutions:
• Delayed Processing: Follow up with the insurance provider to ensure timely processing. • Denied Requests: Review the form for accuracy and completeness, and resubmit with additional information if necessary. • Lack of Communication: Establish clear communication channels with the insurance provider and requesting physician.
Best Practices for Healthcare Providers

To ensure a successful prior authorization process, healthcare providers should follow these best practices:
• Verify patient eligibility and coverage before submitting the form • Use the correct procedure and diagnosis codes • Provide clear and concise clinical information • Attach all required supporting documentation • Establish clear communication channels with the insurance provider and requesting physician
Conclusion
The FEP Prior Auth Form is a crucial document in the prior authorization process, ensuring that patients receive the necessary care while adhering to insurance provider rules and regulations. By following the step-by-step guide and best practices outlined in this article, healthcare providers can streamline the prior authorization process, reducing administrative burden and improving patient outcomes.
We hope this article has provided valuable insights into the FEP Prior Auth Form and its importance in the healthcare industry. If you have any questions or comments, please feel free to share them below.
What is the purpose of the FEP Prior Auth Form?
+The FEP Prior Auth Form is used to request prior authorization for medical procedures, ensuring that insurance providers cover the costs.
What information is required to complete the FEP Prior Auth Form?
+The form requires patient information, policy information, procedure information, diagnosis information, and requesting physician information.
What are some common challenges during the prior authorization process?
+Common challenges include delayed processing, denied requests, and lack of communication.