The authorization process for healthcare services can be a daunting task, especially when dealing with a large insurance provider like Blue Cross Highmark. The complexity of the process can lead to frustration, delays, and even denied claims. However, there are ways to simplify the Blue Cross Highmark authorization process, making it easier for healthcare providers and patients to navigate.

Understanding the Blue Cross Highmark Authorization Process
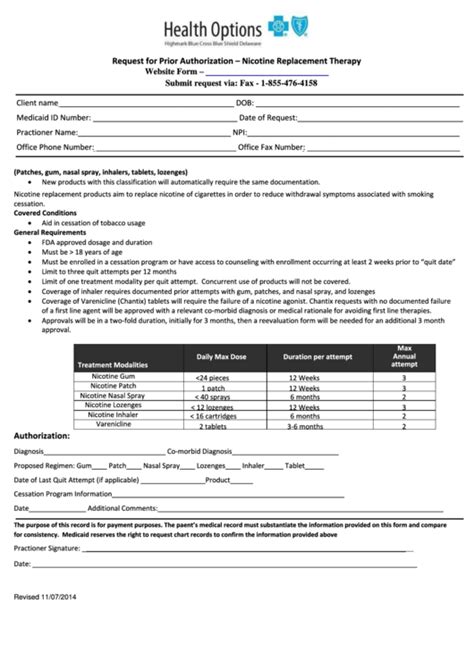
Before we dive into the ways to simplify the authorization process, it's essential to understand how it works. Blue Cross Highmark requires pre-authorization for certain medical services, including surgeries, hospital stays, and specialty treatments. The process involves submitting a request to Blue Cross Highmark, providing detailed information about the patient's condition, treatment plan, and medical history.
5 Ways to Simplify Blue Cross Highmark Authorization
1. Streamline Your Documentation
One of the most significant challenges in the authorization process is gathering and submitting the required documentation. To simplify this step, make sure you have all the necessary documents ready, including:
- Patient's medical history and diagnosis
- Treatment plan and justification
- Test results and medical records
- Prescriptions and medication lists

2. Utilize Electronic Authorization Platforms
Blue Cross Highmark offers electronic authorization platforms, such as the Availity Portal, to simplify the submission process. These platforms allow you to submit requests, track the status, and receive notifications electronically. This can significantly reduce the administrative burden and minimize errors.
Benefits of Electronic Authorization Platforms
- Reduced paperwork and administrative tasks
- Faster submission and processing times
- Improved accuracy and reduced errors
- Enhanced visibility and tracking capabilities
3. Leverage Blue Cross Highmark's Authorization Tools
Blue Cross Highmark provides various tools and resources to help healthcare providers navigate the authorization process. These tools include:
- Authorization guidelines and checklists
- Pre-authorization request forms
- Online portal for submitting and tracking requests
- Customer service support for assistance with the process

4. Develop a Relationship with Blue Cross Highmark Representatives
Building a relationship with Blue Cross Highmark representatives can go a long way in simplifying the authorization process. By establishing open communication channels, you can:
- Clarify requirements and reduce errors
- Receive timely feedback and updates on the status of your requests
- Address any issues or concerns promptly
Benefits of Building a Relationship with Blue Cross Highmark Representatives
- Improved communication and collaboration
- Reduced misunderstandings and errors
- Enhanced trust and credibility
5. Stay Up-to-Date with Blue Cross Highmark's Authorization Requirements
Blue Cross Highmark's authorization requirements can change frequently, and it's essential to stay informed about these updates. By regularly reviewing the Blue Cross Highmark website, attending webinars, and participating in training sessions, you can:
- Stay current with changing requirements and guidelines
- Avoid delays and denials due to non-compliance
- Improve your overall understanding of the authorization process

In Conclusion
Simplifying the Blue Cross Highmark authorization process requires a combination of understanding the process, leveraging available tools and resources, and building relationships with representatives. By implementing these strategies, healthcare providers can reduce administrative burdens, minimize errors, and improve the overall efficiency of the authorization process.
What is the Blue Cross Highmark authorization process?
+The Blue Cross Highmark authorization process involves submitting a request to Blue Cross Highmark for pre-authorization of certain medical services, including surgeries, hospital stays, and specialty treatments.
What documents are required for Blue Cross Highmark authorization?
+The required documents for Blue Cross Highmark authorization include patient's medical history and diagnosis, treatment plan and justification, test results and medical records, and prescriptions and medication lists.
How can I simplify the Blue Cross Highmark authorization process?
+To simplify the Blue Cross Highmark authorization process, you can streamline your documentation, utilize electronic authorization platforms, leverage Blue Cross Highmark's authorization tools, develop a relationship with Blue Cross Highmark representatives, and stay up-to-date with Blue Cross Highmark's authorization requirements.