The prior authorization process for healthcare services can be a daunting and time-consuming task for healthcare providers and patients alike. The Blue Cross Blue Shield of Texas (BCBSTX) prior authorization form is no exception. However, there are ways to simplify the process and reduce the administrative burden. In this article, we will explore five ways to simplify the BCBSTX prior authorization form.
Understanding the Importance of Prior Authorization
Prior authorization is a crucial step in the healthcare process that ensures patients receive necessary and covered treatments while also controlling healthcare costs. However, the process can be complex and time-consuming, leading to delays in patient care and increased administrative costs for healthcare providers.
Simplifying the BCBSTX Prior Authorization Form
1. Electronic Submission
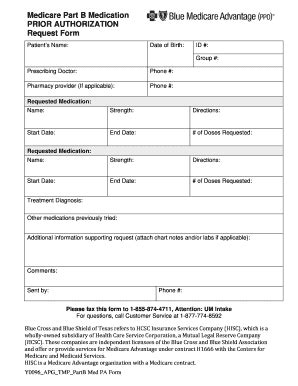
One way to simplify the BCBSTX prior authorization form is to submit it electronically. BCBSTX offers an electronic prior authorization submission system that allows healthcare providers to submit requests online. This reduces the need for paper forms and faxing, making the process faster and more efficient.

By submitting prior authorization requests electronically, healthcare providers can also reduce errors and improve the accuracy of the information submitted.
2. Pre-Authorization Lists
Another way to simplify the BCBSTX prior authorization form is to use pre-authorization lists. BCBSTX provides a list of services and medications that require prior authorization. By reviewing this list, healthcare providers can determine which services and medications require prior authorization and prepare the necessary documentation in advance.

Using pre-authorization lists can help reduce the administrative burden and ensure that prior authorization requests are submitted accurately and efficiently.
3. Clinical Edit Criteria
BCBSTX uses clinical edit criteria to evaluate prior authorization requests. By understanding these criteria, healthcare providers can ensure that prior authorization requests meet the necessary requirements, reducing the likelihood of denials or delays.

Clinical edit criteria include specific medical necessity criteria, treatment guidelines, and other requirements that must be met for prior authorization to be approved.
4. Delegated Credentialing
Delegated credentialing is another way to simplify the BCBSTX prior authorization form. Delegated credentialing allows healthcare providers to delegate the prior authorization process to a third-party vendor. This can help reduce the administrative burden and ensure that prior authorization requests are submitted accurately and efficiently.

By delegating credentialing, healthcare providers can focus on patient care while the third-party vendor handles the prior authorization process.
5. Provider Education
Finally, provider education is key to simplifying the BCBSTX prior authorization form. BCBSTX offers educational resources and training programs to help healthcare providers understand the prior authorization process and requirements.

By educating healthcare providers on the prior authorization process, BCBSTX can help reduce errors and improve the accuracy of prior authorization requests.
Call to Action
Simplifying the BCBSTX prior authorization form requires a combination of electronic submission, pre-authorization lists, clinical edit criteria, delegated credentialing, and provider education. By implementing these strategies, healthcare providers can reduce the administrative burden and ensure that patients receive necessary and covered treatments in a timely manner.
FAQ Section
What is the purpose of prior authorization?
+Prior authorization is a process that ensures patients receive necessary and covered treatments while controlling healthcare costs.
How can I simplify the BCBSTX prior authorization form?
+You can simplify the BCBSTX prior authorization form by using electronic submission, pre-authorization lists, clinical edit criteria, delegated credentialing, and provider education.
What is delegated credentialing?
+Delegated credentialing is a process that allows healthcare providers to delegate the prior authorization process to a third-party vendor.