The healthcare landscape can be overwhelming, especially when it comes to navigating insurance processes. One such process is prior authorization, which is often required by insurance providers before they cover certain treatments or medications. For members of BlueCross BlueShield of Tennessee (BCBST), understanding the prior authorization process is crucial to ensure seamless healthcare experiences. Here, we'll break down the BCBST prior authorization form into 5 easy steps, aiming to simplify the process and empower patients to take control of their healthcare.
Understanding Prior Authorization
Prior authorization is a process used by insurance companies to determine whether a prescribed treatment or medication is medically necessary and covered under the patient's insurance plan. This process is designed to ensure that patients receive safe and effective treatments while minimizing unnecessary healthcare expenses. For BCBST members, prior authorization may be required for certain services, including prescription medications, surgical procedures, and specialist consultations.

Step 1: Determine If Prior Authorization Is Required
Before starting the prior authorization process, it's essential to determine if it's required for your specific treatment or medication. BCBST members can check their insurance plan documents or contact their healthcare provider to confirm whether prior authorization is needed. Additionally, patients can visit the BCBST website to search for specific medications or treatments that require prior authorization.
Steps to Complete the BCBST Prior Authorization Form
Once you've determined that prior authorization is required, follow these 5 easy steps to complete the BCBST prior authorization form:
Step 2: Gather Required Information and Documents
To initiate the prior authorization process, you'll need to gather relevant information and documents. This may include:
- Patient demographics (name, date of birth, etc.)
- Insurance information (policy number, etc.)
- Treatment or medication details (dosage, frequency, etc.)
- Medical records and test results (if applicable)
- Prescription or treatment order from your healthcare provider

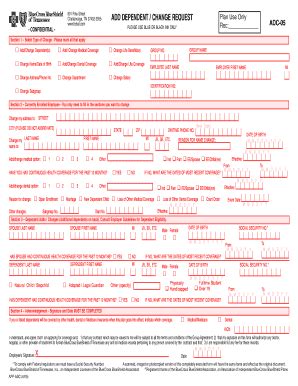
Step 3: Complete the Prior Authorization Form
The BCBST prior authorization form can be obtained from the BCBST website or by contacting your healthcare provider. Complete the form accurately and thoroughly, ensuring that all required information is provided. If you're unsure about any section of the form, don't hesitate to reach out to your healthcare provider or BCBST customer support.
Step 4: Submit the Prior Authorization Form
Once the form is complete, submit it to BCBST along with any required supporting documents. You can submit the form via fax, mail, or online through the BCBST website. Be sure to keep a record of your submission, including the date and method of submission.

Step 5: Follow Up on Your Prior Authorization Request
After submitting your prior authorization form, it's essential to follow up on your request. You can check the status of your request by contacting BCBST customer support or by logging into your online account. If your request is approved, you'll receive notification from BCBST, and your treatment or medication will be covered according to your insurance plan.

By following these 5 easy steps, BCBST members can navigate the prior authorization process with confidence. Remember to stay informed, ask questions, and seek support when needed to ensure a smooth healthcare experience.
Empowering Patients Through Prior Authorization
Prior authorization may seem like a daunting process, but it's designed to ensure that patients receive safe and effective treatments. By understanding the prior authorization process and taking proactive steps, patients can empower themselves to take control of their healthcare. Don't hesitate to reach out to your healthcare provider or BCBST customer support if you have any questions or concerns.

Moving Forward with Confidence
By breaking down the BCBST prior authorization form into 5 easy steps, we hope to have simplified the process and empowered patients to take control of their healthcare. Remember to stay informed, ask questions, and seek support when needed. With confidence and knowledge, you can navigate the prior authorization process and focus on what matters most – your health and well-being.

Your Turn to Share
Have you navigated the prior authorization process with BCBST or another insurance provider? Share your experiences, tips, and advice in the comments below. Your insights can help others feel more confident and empowered in their healthcare journeys.
What is prior authorization, and why is it required?
+Prior authorization is a process used by insurance companies to determine whether a prescribed treatment or medication is medically necessary and covered under the patient's insurance plan.
How do I determine if prior authorization is required for my treatment or medication?
+BCBST members can check their insurance plan documents or contact their healthcare provider to confirm whether prior authorization is needed.
What information and documents are required to complete the BCBST prior authorization form?
+Required information and documents may include patient demographics, insurance information, treatment or medication details, and medical records and test results (if applicable).