Allwell Medicare is a popular Medicare Advantage plan that offers comprehensive coverage to its beneficiaries. As with any Medicare plan, certain services and treatments may require prior authorization to ensure that they are medically necessary and align with the plan's guidelines. In this article, we will delve into the world of Allwell Medicare outpatient authorization forms, providing a comprehensive guide to help healthcare providers and patients navigate the process.
Why is Prior Authorization Important?
Prior authorization is a critical step in the healthcare process that ensures patients receive medically necessary treatments while also controlling healthcare costs. By reviewing the medical necessity of a service or treatment, Allwell Medicare can determine whether it is covered under the patient's plan. This process also helps to reduce unnecessary medical procedures, which can lead to better health outcomes and lower costs for patients and the healthcare system as a whole.

What is the Allwell Medicare Outpatient Authorization Form?
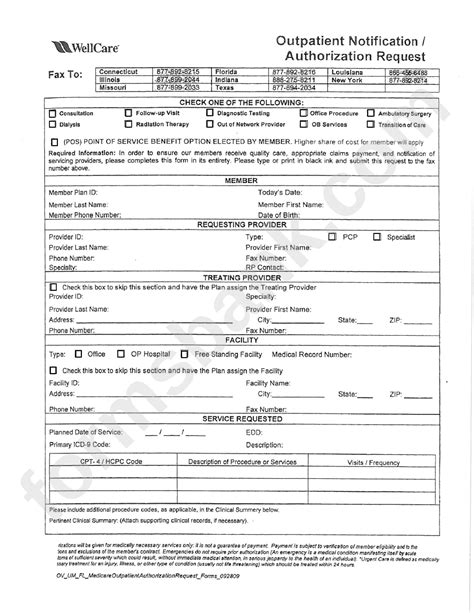
The Allwell Medicare outpatient authorization form is a document that healthcare providers must complete and submit to Allwell Medicare before performing certain outpatient services or treatments. The form requires detailed information about the patient's condition, the proposed treatment, and the medical necessity of the service. By completing this form, healthcare providers can ensure that they have obtained the necessary authorization before proceeding with the treatment.
What Information is Required on the Form?
The Allwell Medicare outpatient authorization form requires the following information:
- Patient's name and Medicare ID number
- Healthcare provider's name and contact information
- Description of the proposed treatment or service
- Medical diagnosis and ICD-10 code
- Treatment plan and duration
- Supporting medical documentation (e.g., lab results, medical records)
How to Complete the Allwell Medicare Outpatient Authorization Form
Completing the Allwell Medicare outpatient authorization form requires careful attention to detail to ensure that all necessary information is provided. Here are some steps to follow:
- Review the plan's guidelines: Before completing the form, review Allwell Medicare's guidelines for prior authorization to ensure that you understand the requirements.
- Gather supporting documentation: Collect any relevant medical records, lab results, or other supporting documentation that demonstrates the medical necessity of the service.
- Complete the form accurately: Fill out the form completely and accurately, ensuring that all required fields are completed.
- Submit the form: Submit the completed form to Allwell Medicare via fax or online portal.

Timeline for Prior Authorization
The timeline for prior authorization may vary depending on the type of service or treatment. Here are some general guidelines:
- Standard requests: 14 calendar days from receipt of the request
- Expedited requests: 72 hours from receipt of the request
- Concurrent reviews: Ongoing during the patient's hospital stay
Common Reasons for Prior Authorization Denials
Prior authorization requests may be denied for several reasons, including:
- Lack of medical necessity: The requested service or treatment is not deemed medically necessary.
- Insufficient documentation: The submitted documentation does not support the medical necessity of the service.
- Non-compliance with plan guidelines: The requested service or treatment does not align with Allwell Medicare's guidelines.
What to Do if a Request is Denied
If a prior authorization request is denied, healthcare providers may appeal the decision by submitting additional information or clarifying the medical necessity of the service.

Best Practices for Healthcare Providers
To ensure a smooth prior authorization process, healthcare providers should:
- Review plan guidelines: Familiarize yourself with Allwell Medicare's guidelines for prior authorization.
- Submit complete requests: Ensure that all required information is provided on the request form.
- Follow up: Verify that the request has been received and is being processed.
Common Challenges and Solutions
- Delays in processing: Submit requests well in advance of the scheduled service or treatment.
- Denials due to lack of documentation: Ensure that all supporting documentation is submitted with the request.

Conclusion
The Allwell Medicare outpatient authorization form is an essential step in the healthcare process that ensures patients receive medically necessary treatments while controlling healthcare costs. By understanding the requirements and following the guidelines outlined in this article, healthcare providers can navigate the prior authorization process with confidence. Remember to review plan guidelines, submit complete requests, and follow up to ensure a smooth process.
We hope this comprehensive guide has been informative and helpful. If you have any further questions or concerns, please don't hesitate to comment below or reach out to Allwell Medicare directly.
What is the purpose of the Allwell Medicare outpatient authorization form?
+The purpose of the form is to ensure that patients receive medically necessary treatments while controlling healthcare costs.
What information is required on the Allwell Medicare outpatient authorization form?
+The form requires patient information, healthcare provider information, description of the proposed treatment, medical diagnosis, and supporting medical documentation.
How long does the prior authorization process take?
+The timeline for prior authorization may vary depending on the type of service or treatment, but standard requests are typically processed within 14 calendar days.