In today's fast-paced healthcare industry, streamlining workflows is crucial for reducing administrative burdens and improving patient care. One of the most significant pain points in medical offices is the prior authorization process. Availity, a leading healthcare technology company, offers a prior authorization form that aims to simplify this process. However, many healthcare professionals struggle to master its use. In this article, we will explore five ways to streamline your workflow and master the Availity prior authorization form.
Understanding the Availity Prior Authorization Form

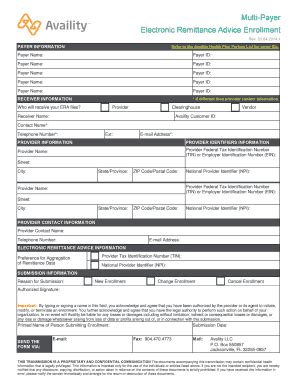
Before diving into the tips, it's essential to understand the basics of the Availity prior authorization form. This form is designed to facilitate the prior authorization process by providing a standardized template for healthcare providers to submit requests to payers. The form typically includes patient demographics, treatment information, and supporting documentation.
Benefits of Using the Availity Prior Authorization Form
Using the Availity prior authorization form can bring several benefits to your medical office, including:
- Reduced administrative burdens: The form's standardized template saves time and effort in preparing prior authorization requests.
- Improved accuracy: The form's built-in validation checks help reduce errors and ensure that all required information is provided.
- Enhanced patient care: Faster processing of prior authorization requests means that patients can receive the necessary treatment more quickly.
Tip 1: Familiarize Yourself with the Availity System

To master the Availity prior authorization form, you need to understand the Availity system's functionality and features. Take some time to explore the system, watch tutorials, and attend webinars to get familiar with its capabilities. This will help you to:
- Navigate the system efficiently
- Understand the prior authorization process
- Identify potential errors and troubleshoot issues
Availity System Features
Some key features of the Availity system include:
- Eligibility and benefits verification
- Prior authorization and referrals
- Claims submission and status tracking
- Patient engagement and communication tools
Tip 2: Use the Availity Form Builder

The Availity form builder is a powerful tool that allows you to create customized prior authorization forms for specific payers and procedures. This feature can help you to:
- Automate the prior authorization process
- Reduce paperwork and administrative burdens
- Improve accuracy and consistency
Form Builder Benefits
Some benefits of using the Availity form builder include:
- Customizable forms for specific payers and procedures
- Automated data population from patient records
- Real-time validation and error checking
Tip 3: Leverage Availity's Integration with EHR Systems

Availity's integration with EHR systems can streamline your workflow by allowing you to access patient information and submit prior authorization requests directly from your EHR system. This integration can help you to:
- Reduce data entry and administrative burdens
- Improve accuracy and consistency
- Enhance patient care and outcomes
EHR Integration Benefits
Some benefits of Availity's EHR integration include:
- Bi-directional data exchange between Availity and EHR systems
- Automated patient data population
- Streamlined prior authorization process
Tip 4: Use Availity's Reporting and Analytics Tools

Availity's reporting and analytics tools can help you to track and analyze prior authorization requests, identify trends, and make data-driven decisions. This feature can help you to:
- Monitor prior authorization request status
- Identify areas for workflow improvement
- Optimize prior authorization processes
Reporting and Analytics Benefits
Some benefits of Availity's reporting and analytics tools include:
- Real-time tracking and analysis of prior authorization requests
- Customizable reports and dashboards
- Data-driven insights for workflow optimization
Tip 5: Stay Up-to-Date with Availity's Training and Support Resources

Finally, it's essential to stay up-to-date with Availity's training and support resources to ensure that you're getting the most out of the prior authorization form. Availity offers various training options, including webinars, tutorials, and on-site training. This can help you to:
- Stay current with system updates and features
- Improve your workflow and productivity
- Enhance patient care and outcomes
Training and Support Benefits
Some benefits of Availity's training and support resources include:
- Expert guidance and support
- Customized training options
- Ongoing education and updates
What is the Availity prior authorization form?
+The Availity prior authorization form is a standardized template for healthcare providers to submit prior authorization requests to payers.
How can I access the Availity system?
+You can access the Availity system through the Availity website or through your EHR system if it's integrated with Availity.
What are the benefits of using the Availity prior authorization form?
+The Availity prior authorization form can help reduce administrative burdens, improve accuracy, and enhance patient care.
By following these five tips, you can master the Availity prior authorization form and streamline your workflow, reducing administrative burdens and improving patient care. Remember to stay up-to-date with Availity's training and support resources to ensure that you're getting the most out of the system. Share your experiences and tips for using the Availity prior authorization form in the comments below.