The world of healthcare can be a complex and overwhelming place, especially when it comes to navigating the intricacies of insurance and medical billing. One crucial aspect of this process is prior authorization, which can help ensure that patients receive the necessary treatments and medications while also controlling healthcare costs. In this article, we will delve into the world of Aultcare prior authorization forms, exploring what they are, why they are necessary, and most importantly, providing a step-by-step guide on how to complete them with ease.
Understanding Aultcare Prior Authorization Forms

Prior authorization is a process used by health insurance companies to determine whether a particular treatment or medication is medically necessary and covered under a patient's insurance plan. Aultcare, a leading healthcare insurance provider, requires prior authorization for certain medical services and prescriptions to ensure that patients receive the most effective and cost-efficient care possible.
Benefits of Prior Authorization
Prior authorization offers several benefits to patients, healthcare providers, and insurance companies alike. Some of the key advantages include:
- Ensures medically necessary care: Prior authorization helps ensure that patients receive treatments and medications that are evidence-based and medically necessary.
- Controls healthcare costs: By reviewing and approving medical services and prescriptions beforehand, prior authorization can help reduce unnecessary healthcare spending.
- Improves patient outcomes: Prior authorization can help patients receive the most effective treatments and medications, leading to better health outcomes.
5 Easy Steps to Complete an Aultcare Prior Authorization Form

Completing an Aultcare prior authorization form may seem daunting, but it can be a straightforward process if you follow these easy steps:
Step 1: Gather Required Information
Before starting the prior authorization process, gather all necessary information, including:
- Patient demographics and insurance information
- Medical records and test results
- Treatment plans and medication lists
- Healthcare provider contact information
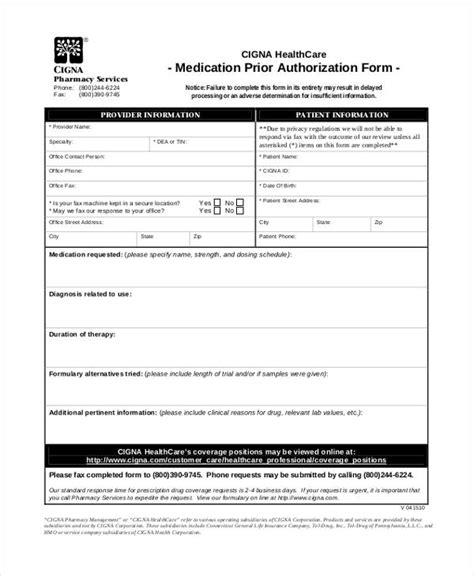
Step 2: Choose the Correct Form
Aultcare offers various prior authorization forms for different medical services and prescriptions. Choose the correct form based on the patient's specific needs.
Step 3: Complete the Form Accurately
Fill out the prior authorization form accurately and completely, ensuring that all required fields are filled in. Be sure to include:
- Patient and healthcare provider information
- Medical diagnosis and treatment plans
- Supporting medical documentation
Step 4: Submit the Form
Submit the completed prior authorization form to Aultcare via fax, email, or online portal. Ensure that all required documentation is included to avoid delays in the review process.
Step 5: Follow Up and Track Status
After submitting the prior authorization form, follow up with Aultcare to track the status of the review process. This can help ensure that the patient receives timely approval and can begin treatment as soon as possible.
Additional Tips and Best Practices

To ensure a smooth prior authorization process, keep the following tips and best practices in mind:
- Submit complete and accurate information to avoid delays
- Include supporting medical documentation to support the request
- Follow up with Aultcare to track the status of the review process
- Keep patients informed throughout the process to manage expectations
Conclusion
Completing an Aultcare prior authorization form may seem like a daunting task, but by following these easy steps and best practices, you can ensure a smooth and efficient process. Remember to gather required information, choose the correct form, complete the form accurately, submit the form, and follow up to track the status. By doing so, you can help patients receive the necessary treatments and medications while controlling healthcare costs.
We encourage you to share your experiences and tips for completing Aultcare prior authorization forms in the comments below. Your feedback can help others navigate this process with ease.
What is prior authorization?
+Prior authorization is a process used by health insurance companies to determine whether a particular treatment or medication is medically necessary and covered under a patient's insurance plan.
Why is prior authorization necessary?
+Prior authorization helps ensure that patients receive the most effective and cost-efficient care possible, while controlling healthcare costs.
How long does the prior authorization process take?
+The prior authorization process typically takes a few days to a week, but can vary depending on the complexity of the request and the efficiency of the submission process.