Varicose veins are a common condition that affects millions of people worldwide. Characterized by enlarged, twisted, and painful veins, varicose veins can significantly impact an individual's quality of life. Aetna, a leading health insurance provider, offers coverage for various treatments, including varicose vein treatment. However, to ensure smooth claims processing, it is essential to understand the precertification form requirements. In this article, we will delve into the 3 precertification form essentials for Aetna varicose vein treatment.
Understanding Aetna's Precertification Process

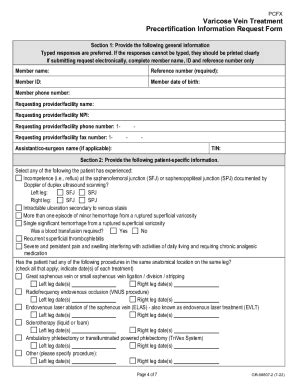
Aetna's precertification process is designed to ensure that patients receive necessary medical treatments while also managing healthcare costs. For varicose vein treatment, Aetna requires healthcare providers to submit a precertification form before performing the procedure. This form helps Aetna determine whether the treatment is medically necessary and meets their coverage criteria.
Essential 1: Patient Information and Medical History
The first essential section of the precertification form requires healthcare providers to furnish detailed patient information and medical history. This includes:
- Patient demographics (name, date of birth, and contact information)
- Medical history, including previous treatments and surgeries
- Current symptoms and diagnosis
- Relevant test results and medical records
Accurate and complete patient information is crucial for Aetna to assess the medical necessity of the varicose vein treatment. Healthcare providers must ensure that they provide all required information to avoid delays or denials in the precertification process.
Varicose Vein Treatment Options and Criteria

Aetna covers various varicose vein treatments, including:
- Endovenous ablation
- Sclerotherapy
- Vein stripping
- Ambulatory phlebectomy
Each treatment option has specific criteria that must be met for Aetna to consider it medically necessary. Healthcare providers must carefully review Aetna's coverage policies and ensure that the chosen treatment aligns with the patient's condition and medical history.
Essential 2: Treatment Plan and Justification
The second essential section of the precertification form requires healthcare providers to outline the proposed treatment plan and provide justification for the chosen treatment. This includes:
- Detailed description of the treatment procedure
- Explanation of why the chosen treatment is medically necessary
- Discussion of alternative treatment options and why they were not selected
Aetna requires healthcare providers to demonstrate that the proposed treatment is the most effective and efficient way to address the patient's varicose vein condition. A clear and concise treatment plan and justification are essential for a successful precertification outcome.
Aetna's Review Process and Timeline

Once the precertification form is submitted, Aetna's review team assesses the request to determine whether the treatment meets their coverage criteria. The review process typically takes 5-10 business days, but may vary depending on the complexity of the case.
Healthcare providers can track the status of the precertification request through Aetna's online portal or by contacting their dedicated customer service representative. It is essential to plan accordingly and allow sufficient time for the review process to avoid delays in treatment.
Essential 3: Supporting Documentation and Additional Information
The third essential section of the precertification form requires healthcare providers to submit supporting documentation and additional information to supplement the request. This may include:
- Medical records and test results
- Photographs or images of the affected area
- Letters of medical necessity or justification
Aetna may request additional information or clarification during the review process. Healthcare providers must be prepared to provide supplementary documentation to support the precertification request.
Conclusion and Next Steps

In conclusion, the Aetna varicose vein treatment precertification form requires healthcare providers to furnish detailed patient information, a treatment plan and justification, and supporting documentation. By understanding these essential components, healthcare providers can ensure a smooth precertification process and timely treatment for their patients.
If you have any questions or concerns about the Aetna varicose vein treatment precertification process, we encourage you to share them in the comments section below. Additionally, if you found this article informative, please share it with your colleagues and friends.
FAQ Section:
What is the purpose of the Aetna precertification form?
+The Aetna precertification form is designed to ensure that patients receive necessary medical treatments while also managing healthcare costs.
What information is required on the precertification form?
+The precertification form requires patient information, medical history, treatment plan, and justification, as well as supporting documentation.
How long does the Aetna review process typically take?
+The Aetna review process typically takes 5-10 business days, but may vary depending on the complexity of the case.