As a healthcare provider, you understand the importance of ensuring that your patients receive the medical attention they need, while also navigating the complex world of insurance claims. Ambetter, a popular health insurance provider, offers a range of plans to individuals and families. However, there may be instances where a claim is denied, and an appeal is necessary. In this article, we will guide you through the 5 steps to filing an Ambetter provider appeal form.
Understanding the Ambetter Appeal Process

Before we dive into the 5 steps, it's essential to understand the Ambetter appeal process. The process typically involves reviewing the initial claim determination, gathering supporting documentation, and submitting the appeal form. Ambetter provides a clear outline of the appeal process on their website, which can be accessed by registered providers.
Why File an Appeal?
Filing an appeal is crucial when a claim is denied, and you believe that the decision was incorrect. An appeal can help to:
- Reconsider the claim determination
- Obtain additional information or clarification
- Resolve any discrepancies or errors
Step 1: Review the Claim Determination

The first step in filing an Ambetter provider appeal form is to review the claim determination. Carefully examine the explanation of benefits (EOB) or the claim determination letter to understand the reason for the denial. Check for any errors or discrepancies in the claim submission, such as incorrect patient information or missing documentation.
Common Reasons for Claim Denial
Some common reasons for claim denial include:
- Lack of medical necessity
- Incorrect coding or billing
- Insufficient documentation
- Pre-existing condition exclusions
Step 2: Gather Supporting Documentation

The next step is to gather supporting documentation to substantiate the claim. This may include:
- Medical records
- Test results
- Treatment plans
- Correspondence with the patient or their representative
Ensure that all documentation is accurate, complete, and relevant to the claim.
Best Practices for Documenting Medical Necessity
When documenting medical necessity, keep the following best practices in mind:
- Clearly explain the patient's condition and treatment plan
- Provide evidence of the patient's symptoms and diagnosis
- Document any relevant medical history or test results
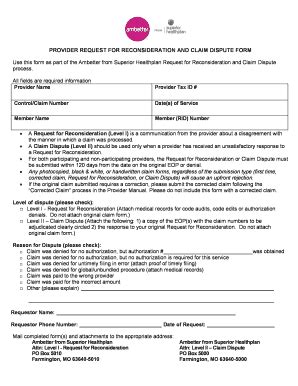
Step 3: Complete the Ambetter Provider Appeal Form

Once you have gathered the necessary documentation, complete the Ambetter provider appeal form. The form can be accessed on the Ambetter website or by contacting their customer service department.
Required Information for the Appeal Form
When completing the appeal form, ensure that you provide the following information:
- Patient's name and member ID
- Claim number or date of service
- Reason for the appeal
- Supporting documentation
Step 4: Submit the Appeal Form and Supporting Documentation

After completing the appeal form, submit it to Ambetter along with the supporting documentation. Ensure that all submissions are made within the required timeframe, typically 180 days from the date of the claim determination.
Submission Options
Ambetter provides several submission options, including:
- Online portal
- Fax
Choose the method that best suits your needs.
Step 5: Follow Up on the Appeal Status

The final step is to follow up on the appeal status. Ambetter will review the appeal and provide a determination within a specified timeframe, typically 30-60 days.
Ambetter Appeal Status
You can check the status of your appeal by:
- Logging into the Ambetter online portal
- Contacting the Ambetter customer service department
- Checking the appeal status on the Ambetter website
By following these 5 steps, you can effectively file an Ambetter provider appeal form and increase the chances of a successful appeal.
We invite you to share your experiences or ask questions about the Ambetter appeal process in the comments section below. Don't forget to share this article with your colleagues and peers who may benefit from this information.
What is the timeframe for submitting an Ambetter appeal?
+Ambetter requires appeals to be submitted within 180 days from the date of the claim determination.
What documentation is required for an Ambetter appeal?
+Ambetter requires supporting documentation, such as medical records, test results, and treatment plans, to substantiate the claim.
How long does it take for Ambetter to review an appeal?
+Ambetter typically reviews appeals within 30-60 days from the date of submission.