The process of obtaining precertification for specialty medications can be a daunting task, especially for healthcare providers and patients navigating the complexities of the healthcare system. Aetna, a leading health insurance provider, has implemented a precertification process to ensure that patients receive the necessary medications while also managing costs and promoting effective treatment. In this article, we will delve into the world of Aetna specialty medication precertification, exploring the process, benefits, and requirements to help healthcare providers and patients better understand and navigate this often-confusing landscape.
Understanding Aetna Specialty Medication Precertification

Aetna specialty medication precertification is a process that requires healthcare providers to obtain approval from Aetna before prescribing certain specialty medications to patients. This process is designed to ensure that patients receive the most effective and cost-efficient treatment for their specific condition. By requiring precertification, Aetna aims to promote the use of evidence-based treatments, reduce healthcare costs, and improve patient outcomes.
Benefits of Aetna Specialty Medication Precertification
The precertification process offers several benefits to healthcare providers, patients, and the healthcare system as a whole. Some of the key benefits include:
- Improved patient outcomes: By ensuring that patients receive the most effective treatment for their condition, precertification helps to improve patient outcomes and reduce the risk of complications.
- Reduced healthcare costs: Precertification helps to reduce healthcare costs by promoting the use of cost-effective treatments and minimizing unnecessary spending on expensive medications.
- Enhanced patient safety: The precertification process helps to minimize the risk of adverse reactions and interactions by ensuring that patients receive medications that are safe and effective for their specific condition.
The Precertification Process: A Step-by-Step Guide

The precertification process for Aetna specialty medications involves several steps, which are outlined below:
- Determine if precertification is required: Healthcare providers must determine if the medication they wish to prescribe requires precertification. Aetna provides a list of medications that require precertification on their website.
- Gather required information: Healthcare providers must gather all necessary information, including the patient's medical history, current treatment plan, and medication regimen.
- Submit a precertification request: Healthcare providers must submit a precertification request to Aetna, either online or by phone. The request must include all required information and supporting documentation.
- Review and approval: Aetna reviews the precertification request and may request additional information or clarification. If approved, Aetna will notify the healthcare provider and the patient.
Required Documentation and Information
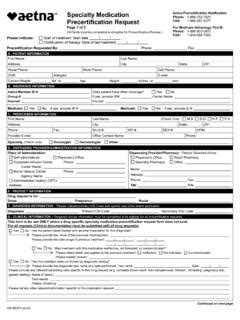
To ensure a smooth precertification process, healthcare providers must provide all required documentation and information, including:
- Patient demographics: Patient name, date of birth, and contact information.
- Medical history: Patient's medical history, including current and past conditions, allergies, and medications.
- Current treatment plan: A detailed description of the patient's current treatment plan, including medications, dosages, and frequency.
- Medication regimen: A list of all medications the patient is currently taking, including dosages and frequency.
- Supporting documentation: Any additional documentation that supports the precertification request, such as lab results, medical records, or physician statements.
Aetna Specialty Medication Precertification Forms and Resources

Aetna provides several forms and resources to help healthcare providers navigate the precertification process. These include:
- Precertification request form: A standard form that healthcare providers can use to submit precertification requests.
- Medication list: A list of medications that require precertification, which can be found on the Aetna website.
- Precertification guidelines: A detailed guide that outlines the precertification process, requirements, and timelines.
Tips for a Successful Precertification Request
To increase the chances of a successful precertification request, healthcare providers should:
- Ensure complete and accurate information: Provide all required information and documentation to avoid delays or denials.
- Submit requests in a timely manner: Submit precertification requests well in advance of the patient's treatment start date.
- Follow up on requests: Follow up with Aetna to ensure that the request is being processed and to address any issues or concerns.
Aetna Specialty Medication Precertification FAQs

We have compiled a list of frequently asked questions (FAQs) to help healthcare providers and patients better understand the Aetna specialty medication precertification process.
What is Aetna specialty medication precertification?
+Aetna specialty medication precertification is a process that requires healthcare providers to obtain approval from Aetna before prescribing certain specialty medications to patients.
What are the benefits of Aetna specialty medication precertification?
+The benefits of Aetna specialty medication precertification include improved patient outcomes, reduced healthcare costs, and enhanced patient safety.
What information is required for a precertification request?
+The required information includes patient demographics, medical history, current treatment plan, medication regimen, and supporting documentation.
By understanding the Aetna specialty medication precertification process, healthcare providers and patients can work together to ensure that patients receive the necessary medications while also managing costs and promoting effective treatment. We hope that this article has provided valuable insights and information to help navigate this complex process. If you have any further questions or concerns, please do not hesitate to reach out to us.
Take Action Today!

Don't let the precertification process hold you back from providing the best possible care for your patients. Take action today by:
- Educating yourself and your staff: Take the time to learn about the Aetna specialty medication precertification process and requirements.
- Staying up-to-date: Stay current with the latest information and updates on the Aetna website and through their provider portal.
- Reaching out to Aetna: Don't hesitate to reach out to Aetna with any questions or concerns you may have about the precertification process.
By taking action today, you can ensure that your patients receive the necessary medications and treatment they need to thrive.