As a healthcare professional, you're likely no stranger to the complexities of prior authorization forms. One such form that may be familiar to you is the Magellan prior authorization form. In this article, we'll delve into the ins and outs of this form, exploring its purpose, benefits, and steps for completion.
The prior authorization process is a critical step in ensuring that patients receive the necessary treatments while also controlling healthcare costs. The Magellan prior authorization form is a crucial document that facilitates this process, providing a standardized framework for healthcare providers to request authorization for specific treatments or services.
Understanding the Magellan Prior Authorization Form

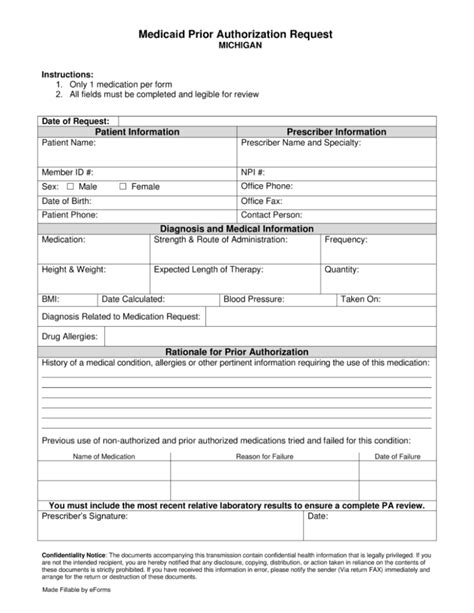
The Magellan prior authorization form is designed to streamline the authorization process, making it easier for healthcare providers to request approval for treatments or services. The form typically includes sections for patient demographics, treatment information, and clinical justification for the requested service.
Key Components of the Magellan Prior Authorization Form
The Magellan prior authorization form typically includes the following key components:
- Patient demographics: This section includes patient information such as name, date of birth, and contact details.
- Treatment information: This section outlines the treatment or service being requested, including the type of treatment, dosage, and frequency.
- Clinical justification: This section provides a detailed explanation of the medical necessity for the requested treatment or service.
Benefits of the Magellan Prior Authorization Form

The Magellan prior authorization form offers several benefits to healthcare providers and patients alike. Some of the key benefits include:
- Streamlined authorization process: The standardized form makes it easier for healthcare providers to request authorization, reducing administrative burdens and delays.
- Improved communication: The form facilitates clear communication between healthcare providers and payers, reducing misunderstandings and miscommunications.
- Enhanced patient care: By ensuring that patients receive the necessary treatments, the Magellan prior authorization form helps to improve patient outcomes and quality of care.
Steps for Completing the Magellan Prior Authorization Form
Completing the Magellan prior authorization form requires careful attention to detail and accurate information. Here are the steps to follow:
- Gather patient information: Collect patient demographics, including name, date of birth, and contact details.
- Determine treatment information: Outline the treatment or service being requested, including the type of treatment, dosage, and frequency.
- Provide clinical justification: Offer a detailed explanation of the medical necessity for the requested treatment or service.
- Review and submit: Review the form carefully and submit it to the payer for authorization.
Common Challenges and Solutions

While the Magellan prior authorization form is designed to streamline the authorization process, challenges may still arise. Some common challenges and solutions include:
- Incomplete or inaccurate information: Ensure that all sections of the form are completed accurately and thoroughly.
- Delays in authorization: Submit the form well in advance of the treatment or service date to allow for timely authorization.
- Denials or rejections: Review the form carefully to ensure that all necessary information is included and resubmit as needed.
Best Practices for Healthcare Providers
To ensure a smooth and efficient prior authorization process, healthcare providers can follow these best practices:
- Use the standardized Magellan prior authorization form to reduce errors and delays.
- Provide clear and concise clinical justification to support the requested treatment or service.
- Submit the form well in advance of the treatment or service date to allow for timely authorization.
Conclusion and Next Steps

In conclusion, the Magellan prior authorization form is a critical document that facilitates the prior authorization process, ensuring that patients receive the necessary treatments while controlling healthcare costs. By understanding the purpose, benefits, and steps for completion, healthcare providers can navigate the prior authorization process with ease.
If you have any questions or concerns about the Magellan prior authorization form, please don't hesitate to reach out to our team. We're here to help.
Take Action Today!
- Share this article with your colleagues and peers to help spread awareness about the Magellan prior authorization form.
- Download a sample Magellan prior authorization form to use as a reference guide.
- Contact our team for assistance with completing the form or navigating the prior authorization process.
What is the purpose of the Magellan prior authorization form?
+The Magellan prior authorization form is designed to facilitate the prior authorization process, ensuring that patients receive the necessary treatments while controlling healthcare costs.
What information is required on the Magellan prior authorization form?
+The form typically includes sections for patient demographics, treatment information, and clinical justification for the requested service.
How can I ensure a smooth and efficient prior authorization process?
+Use the standardized Magellan prior authorization form, provide clear and concise clinical justification, and submit the form well in advance of the treatment or service date.