For patients diagnosed with osteoporosis or bone-related disorders, Prolia (denosumab) is a crucial medication that can help prevent bone fractures and reduce the risk of complications. However, many insurance providers, including Aetna, require prior authorization before covering the cost of Prolia. In this article, we will guide you through the 5 easy steps to complete an Aetna Prolia prior authorization, ensuring that you or your loved ones receive the necessary treatment without any hassle.
Understanding the Importance of Prior Authorization

Prior authorization is a process used by insurance providers to determine whether a specific treatment or medication is medically necessary and covered under the patient's insurance plan. This process helps to ensure that patients receive the most effective and cost-efficient treatment for their condition. For patients requiring Prolia, prior authorization is typically required to verify that the medication is necessary and that the patient meets the specified criteria for coverage.
Step 1: Gather Required Documents and Information

To initiate the prior authorization process, you will need to gather the required documents and information. These typically include:
- Patient's medical records, including diagnosis and treatment history
- Prescription for Prolia from a licensed healthcare provider
- Patient's insurance card and identification
- Contact information for the patient's healthcare provider
Additional Requirements
Aetna may also require additional information, such as:
- Documentation of previous treatments and their outcomes
- Results of relevant laboratory tests or imaging studies
- Information about the patient's medical history, including any allergies or sensitivities
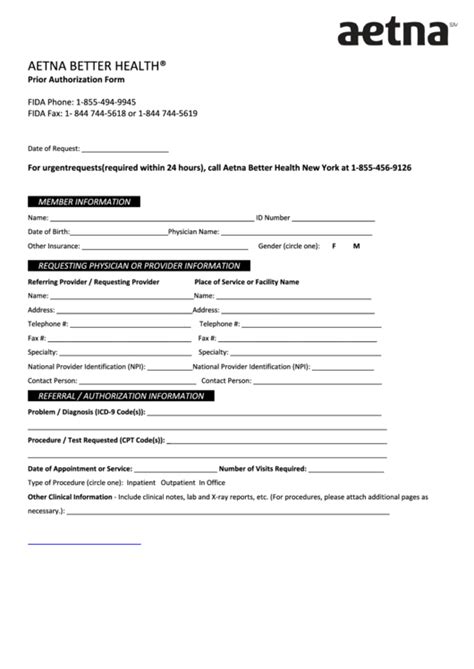
Step 2: Submit the Prior Authorization Request

Once you have gathered all the necessary documents and information, you can submit the prior authorization request to Aetna. You can do this online through the Aetna provider portal or by mail/fax using the prior authorization form. Be sure to follow the instructions carefully and provide all the required information to avoid delays.
Submission Methods
Aetna offers various submission methods, including:
- Online portal: Aetna's online portal allows you to submit prior authorization requests electronically.
- Mail: You can submit the prior authorization request by mail to the address specified on the form.
- Fax: You can also submit the request by fax to the number specified on the form.
Step 3: Wait for Aetna's Review and Decision

After submitting the prior authorization request, Aetna will review the information and make a decision regarding coverage. This process typically takes a few days to a week, but it may take longer in some cases. You can check the status of the request online or by contacting Aetna's customer service.
Decision Outcomes
Aetna's decision may result in one of the following outcomes:
- Approval: Prolia is covered, and the patient can begin treatment.
- Denial: Prolia is not covered, and the patient may need to explore alternative treatment options.
- Request for additional information: Aetna may request additional information to make a decision.
Step 4: Respond to Aetna's Decision

If Aetna denies the prior authorization request or requests additional information, you can respond to their decision. This may involve providing additional documentation or information to support the request. If the request is denied, you can also appeal the decision.
Appeal Process
Aetna's appeal process typically involves the following steps:
- Submitting an appeal request in writing
- Providing additional information or documentation to support the appeal
- Waiting for Aetna's review and decision
Step 5: Receive Approval and Begin Treatment

If Aetna approves the prior authorization request, the patient can begin treatment with Prolia. Be sure to follow the treatment plan and schedule follow-up appointments as recommended by the healthcare provider.
Importance of Adherence
Adhering to the treatment plan is crucial to ensure the effectiveness of Prolia. Patients should take the medication as directed and attend follow-up appointments to monitor their condition.
By following these 5 easy steps, you can complete the Aetna Prolia prior authorization process and ensure that you or your loved ones receive the necessary treatment for osteoporosis or bone-related disorders.
What is prior authorization, and why is it required?
+Prior authorization is a process used by insurance providers to determine whether a specific treatment or medication is medically necessary and covered under the patient's insurance plan.
What information is required for an Aetna Prolia prior authorization?
+Aetna typically requires the patient's medical records, prescription for Prolia, insurance card and identification, and contact information for the healthcare provider.
How long does the prior authorization process take?
+The prior authorization process typically takes a few days to a week, but it may take longer in some cases.