The world of healthcare insurance can be overwhelming, especially when dealing with denied claims or disputed coverage. As a policyholder, it's essential to understand the appeals process to ensure you receive the benefits you're entitled to. In this article, we'll delve into the Highmark appeal form, providing a step-by-step guide to help you navigate the process with ease.
Highmark, a leading health insurance provider, has a well-established appeals process in place to address policyholder concerns. The appeals process allows you to dispute a denied claim or coverage decision, ensuring that your voice is heard and your benefits are protected. Understanding the Highmark appeal form and the associated process is crucial to successfully resolving disputes and receiving the coverage you need.
Understanding the Highmark Appeal Form

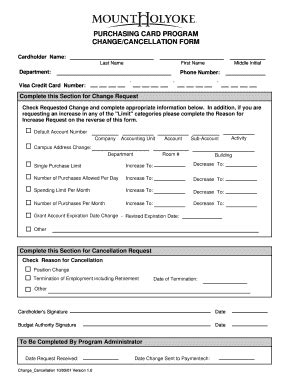
The Highmark appeal form is a standardized document used to initiate the appeals process. The form requires you to provide detailed information about the disputed claim or coverage decision, including your policy details, the denied claim, and the reasons for appealing. It's essential to complete the form accurately and thoroughly to ensure your appeal is processed efficiently.
Components of the Highmark Appeal Form
The Highmark appeal form typically consists of the following components:
- Policyholder information: Your name, policy number, and contact details.
- Claim information: The denied claim or coverage decision, including the claim number and date of service.
- Reason for appeal: A clear explanation of why you're disputing the denied claim or coverage decision.
- Supporting documentation: Any relevant medical records, bills, or correspondence that support your appeal.
The Appeals Process: A Step-by-Step Guide

The Highmark appeals process involves several steps, each designed to ensure that your concerns are thoroughly reviewed and addressed. Here's a step-by-step guide to help you navigate the process:
Step 1: Review the Denied Claim or Coverage Decision
Carefully review the denied claim or coverage decision to understand the reasons behind the denial. Check for any errors or inconsistencies in the decision-making process.
Step 2: Gather Supporting Documentation
Collect any relevant medical records, bills, or correspondence that support your appeal. Ensure that all documentation is accurate and up-to-date.
Step 3: Complete the Highmark Appeal Form
Complete the Highmark appeal form, providing all required information and supporting documentation. Ensure that the form is signed and dated.
Step 4: Submit the Appeal
Submit the completed appeal form and supporting documentation to Highmark via mail, fax, or online portal. Ensure that you retain a copy of the appeal form and supporting documentation for your records.
Step 5: Review and Response
Highmark will review your appeal and respond with a determination. If your appeal is approved, your claim will be reprocessed, and you'll receive the necessary benefits. If your appeal is denied, you'll receive an explanation of the decision and information on further appeal options.
Additional Tips and Considerations

- Ensure that you submit your appeal within the specified timeframe (usually 180 days from the date of the denied claim or coverage decision).
- Keep detailed records of your appeal, including dates, times, and correspondence.
- If you're unsure about the appeals process or need assistance, contact Highmark's customer service or a licensed insurance professional.
- Consider seeking professional help if you're dealing with a complex or high-stakes appeal.
Conclusion
The Highmark appeal form is an essential tool for policyholders to dispute denied claims or coverage decisions. By understanding the appeals process and following the step-by-step guide outlined above, you can effectively navigate the system and ensure that your benefits are protected. Remember to stay informed, keep detailed records, and seek professional help when needed.
We invite you to share your experiences or ask questions about the Highmark appeal form and process in the comments section below. Your feedback and insights will help others navigate this complex process.
What is the deadline for submitting a Highmark appeal?
+The deadline for submitting a Highmark appeal is typically 180 days from the date of the denied claim or coverage decision.
Can I appeal a denied claim multiple times?
+Yes, you can appeal a denied claim multiple times, but each appeal must be based on new or additional information not previously submitted.
How long does the Highmark appeal process typically take?
+The Highmark appeal process typically takes 30-60 days, but may vary depending on the complexity of the appeal and the volume of appeals being processed.