Receiving approval for Aetna Ocrevus PA form can be a challenging and time-consuming process, especially for patients who are in dire need of the medication. Ocrevus (ocrelizumab) is a life-changing treatment for multiple sclerosis (MS) and other autoimmune diseases. However, prior authorization (PA) requirements can delay access to this essential medication. In this article, we will explore five valuable tips to increase the chances of Aetna Ocrevus PA form approval, ensuring that patients receive the treatment they need in a timely manner.
Understanding Aetna's Prior Authorization Requirements

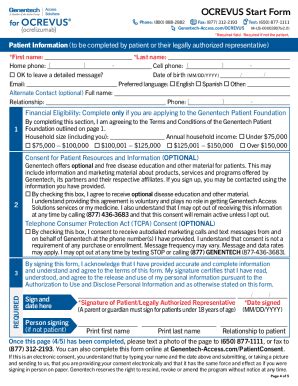
Before we dive into the tips, it's essential to understand Aetna's prior authorization requirements for Ocrevus. Aetna, like many other insurance providers, requires a PA to ensure that the medication is medically necessary and cost-effective. The PA process involves submitting a request to Aetna, which includes providing medical records, test results, and other relevant documentation to support the patient's need for Ocrevus.
Tip 1: Verify Patient Eligibility and Coverage
The first step in increasing the chances of Aetna Ocrevus PA form approval is to verify patient eligibility and coverage. Ensure that the patient has an active Aetna insurance policy that covers Ocrevus. Check the policy's terms and conditions to confirm that the patient meets the eligibility criteria. Additionally, verify that the prescribing physician is part of Aetna's network to avoid any potential issues with coverage.
Gathering Required Documentation

To support the PA request, it's crucial to gather all required documentation. This typically includes:
- Medical records, including diagnosis, medical history, and treatment plans
- Test results, such as MRI or laboratory reports
- Medication history, including previous treatments and their outcomes
- A letter of medical necessity from the prescribing physician
Tip 2: Ensure Accurate and Complete Documentation
Accuracy and completeness are vital when submitting documentation for Aetna Ocrevus PA form approval. Double-check that all required documents are included, and ensure that they are accurate and up-to-date. Incomplete or inaccurate documentation can lead to delays or even denial of the PA request.
Submitting the Prior Authorization Request

Once all required documentation is gathered, submit the PA request to Aetna. Ensure that the request is submitted through the correct channel, such as Aetna's online portal or fax. Follow up with Aetna to confirm receipt of the request and to inquire about the status of the review process.
Tip 3: Follow Up with Aetna
Following up with Aetna is crucial to ensure that the PA request is being processed in a timely manner. If there are any issues or concerns, Aetna may contact the prescribing physician or the patient's representative for additional information. Be prepared to provide any necessary documentation or clarification to support the PA request.
Appealing a Denied Prior Authorization Request

If the PA request is denied, it's essential to understand the reason for the denial and to appeal the decision if necessary. Aetna provides a clear explanation of the denial, including the specific criteria that were not met. Use this information to appeal the decision, providing additional documentation or clarification to support the PA request.
Tip 4: Understand the Appeals Process
The appeals process can be complex and time-consuming. Understand the specific steps involved in appealing a denied PA request, including the submission of additional documentation and the review process. Be prepared to provide any necessary information to support the appeal.
The Importance of Timely Reauthorization

Ocrevus is typically administered via infusion every six months. To ensure uninterrupted treatment, it's essential to reauthorize the medication before the current authorization expires. Aetna requires a reauthorization request to be submitted at least 30 days before the current authorization expires.
Tip 5: Plan Ahead for Reauthorization
Plan ahead for reauthorization by submitting the request well in advance of the expiration date. Ensure that all required documentation is up-to-date and accurate to avoid any potential delays. Aetna may request additional information or clarification during the reauthorization process.
In conclusion, receiving approval for Aetna Ocrevus PA form requires a thorough understanding of the prior authorization process, accurate and complete documentation, and timely follow-up. By following these five valuable tips, patients and healthcare providers can increase the chances of approval and ensure that essential treatment is received in a timely manner.
We encourage you to share your experiences with Aetna Ocrevus PA form approval in the comments section below. Your feedback can help others navigate the prior authorization process and access the treatment they need.
What is the typical turnaround time for Aetna Ocrevus PA form approval?
+The typical turnaround time for Aetna Ocrevus PA form approval is 5-10 business days. However, this timeframe may vary depending on the complexity of the request and the availability of required documentation.
Can I appeal a denied Aetna Ocrevus PA form?
+Yes, you can appeal a denied Aetna Ocrevus PA form. Aetna provides a clear explanation of the denial, including the specific criteria that were not met. Use this information to appeal the decision, providing additional documentation or clarification to support the PA request.
How often do I need to reauthorize Ocrevus with Aetna?
+Ocrevus is typically administered via infusion every six months. To ensure uninterrupted treatment, Aetna requires a reauthorization request to be submitted at least 30 days before the current authorization expires.