As a medical professional, you understand the importance of streamlining administrative tasks to focus on what matters most – providing quality patient care. One crucial aspect of this is navigating prior authorization processes, which can be complex and time-consuming. In this article, we'll delve into the Aetna Inflectra prior authorization form, providing a comprehensive guide to help you efficiently manage this process.
Understanding the Need for Prior Authorization
Prior authorization is a requirement by health insurance providers, including Aetna, to ensure that certain medications, treatments, or services are medically necessary before they are covered. This process aims to control healthcare costs, prevent unnecessary treatments, and ensure that patients receive evidence-based care.
Inflectra, a biosimilar medication, is used to treat various autoimmune diseases, such as rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis. Given its high cost, Aetna requires prior authorization to ensure that its use is justified and aligns with established clinical guidelines.

The Aetna Inflectra Prior Authorization Form: A Step-by-Step Guide
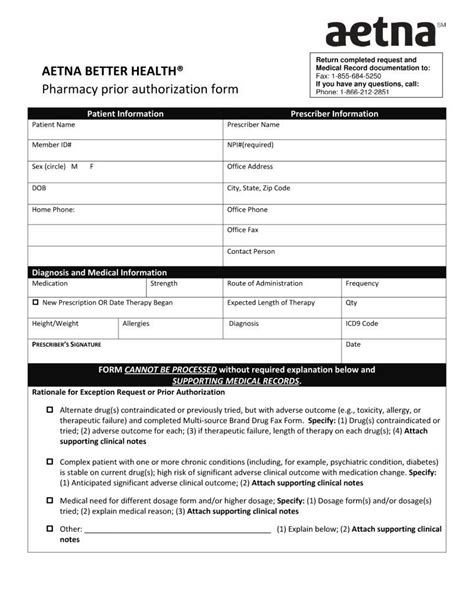
To obtain prior authorization for Inflectra, you'll need to submit a comprehensive request to Aetna. Here's a step-by-step guide to help you navigate this process:
- Gather Required Information: Before starting the prior authorization process, ensure you have the following information readily available:
- Patient demographics and contact information
- Medical history, including diagnoses and treatment plans
- Current medication list
- Laboratory results and relevant medical records
- Determine the Appropriate Form: Aetna offers various prior authorization forms for different medications and services. Ensure you're using the correct form for Inflectra.
- Complete the Form: Fill out the prior authorization form accurately and thoroughly. Be prepared to provide detailed information about the patient's medical condition, treatment plan, and justification for using Inflectra.
- Attach Supporting Documentation: Include all relevant medical records, laboratory results, and other supporting documentation to justify the use of Inflectra.
- Submit the Request: Fax or mail the completed prior authorization form and supporting documentation to Aetna.
Aetna Inflectra Prior Authorization Form Requirements
When completing the prior authorization form, pay close attention to the following requirements:
- Patient Information: Ensure accurate and complete patient demographics, including name, date of birth, and contact information.
- Clinical Information: Provide detailed information about the patient's medical condition, including diagnosis, symptoms, and treatment history.
- Treatment Plan: Outline the treatment plan, including the proposed use of Inflectra, dosage, and duration of therapy.
- Justification: Clearly justify the use of Inflectra, citing relevant clinical guidelines and medical literature.

Streamlining the Prior Authorization Process
To minimize delays and reduce the administrative burden, consider the following strategies:
- Electronic Submission: Aetna offers electronic prior authorization submission options, which can reduce processing time and improve accuracy.
- Pre-Authorization Check: Verify patient eligibility and benefits before submitting the prior authorization request.
- Real-Time Updates: Monitor the status of your prior authorization requests through Aetna's online portal or mobile app.
Common Challenges and Solutions
Be prepared to address common challenges that may arise during the prior authorization process:
- Incomplete or Inaccurate Information: Ensure accurate and complete information to avoid delays or denials.
- Insufficient Justification: Provide clear and compelling justification for the use of Inflectra, citing relevant clinical guidelines and medical literature.
- Denials or Appeals: Understand Aetna's appeal process and be prepared to resubmit or appeal denied requests.

Conclusion
The Aetna Inflectra prior authorization form is a crucial step in ensuring that patients receive necessary treatments while controlling healthcare costs. By understanding the prior authorization process, gathering required information, and completing the form accurately, you can efficiently manage this process and improve patient outcomes.

Now that you've learned how to navigate the Aetna Inflectra prior authorization form, share your experiences and tips with colleagues to help streamline administrative tasks and enhance patient care.
Your Turn: Share your thoughts and questions about the Aetna Inflectra prior authorization form in the comments section below.
What is the purpose of prior authorization?
+Prior authorization is a process used by health insurance providers to ensure that certain medications, treatments, or services are medically necessary before they are covered.
How do I submit a prior authorization request to Aetna?
+Aetna accepts prior authorization requests via fax, mail, or electronic submission. Ensure you use the correct form and include all required information and supporting documentation.
What happens if my prior authorization request is denied?
+If your prior authorization request is denied, you can appeal the decision by resubmitting the request with additional information or by contacting Aetna's appeals department.