The world of healthcare can be complex and overwhelming, especially when it comes to navigating the process of prior authorization for medications like Entyvio. For patients and healthcare providers, understanding the steps involved in obtaining prior authorization from insurance companies like Aetna is crucial to ensure timely access to necessary treatments. In this article, we will break down the 5 essential steps to Aetna Entyvio prior authorization, providing you with a comprehensive guide to simplify the process.
Understanding the Importance of Prior Authorization
Prior authorization is a process used by health insurance companies to determine whether a particular medication or treatment is medically necessary for a patient. This process helps control costs and ensure that patients receive the most effective and safe treatments. For medications like Entyvio, which is used to treat ulcerative colitis and Crohn's disease, prior authorization is often required due to its high cost and potential side effects.
Step 1: Verify Patient Eligibility and Benefits
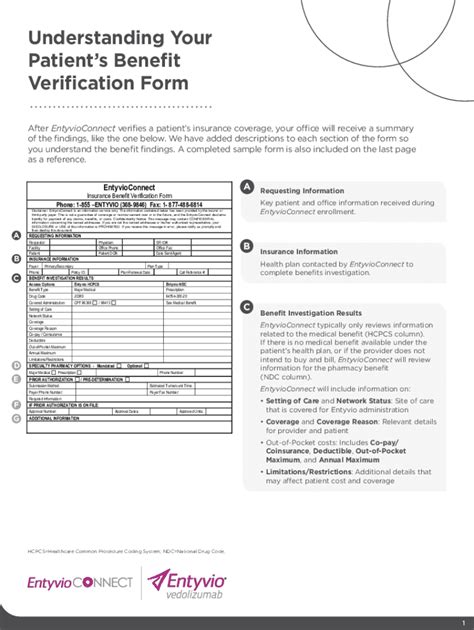
The first step in the prior authorization process is to verify the patient's eligibility and benefits. This involves checking the patient's insurance coverage to ensure that Entyvio is covered under their plan. Healthcare providers can contact Aetna directly to verify the patient's eligibility and benefits. This step is crucial in determining whether the patient's insurance plan covers the medication and what out-of-pocket costs they may be responsible for.

Step 2: Gather Required Documentation
The second step is to gather all required documentation to support the prior authorization request. This typically includes:
- Patient demographics and medical history
- Diagnosis and treatment plan
- Lab results and medical records
- Previous treatment attempts and responses
- Relevant medical literature or clinical guidelines
Healthcare providers should ensure that all documentation is accurate, complete, and up-to-date to avoid delays or denials.
What to Include in the Documentation
- A clear diagnosis and treatment plan
- Documentation of previous treatment attempts and responses
- Lab results and medical records that support the diagnosis and treatment plan
- Relevant medical literature or clinical guidelines that support the use of Entyvio
Step 3: Submit the Prior Authorization Request
Once all required documentation is gathered, the healthcare provider can submit the prior authorization request to Aetna. This can typically be done online, by phone, or by fax. The request should include all relevant documentation and information to support the request.

Step 4: Follow-up and Respond to Additional Requests
After submitting the prior authorization request, the healthcare provider should follow up with Aetna to ensure that the request is being processed. Aetna may request additional information or documentation to support the request. The healthcare provider should respond promptly to these requests to avoid delays or denials.
Tips for Following up
- Follow up with Aetna within 3-5 business days after submitting the request
- Respond promptly to additional requests for information or documentation
- Keep a record of all communication with Aetna, including dates and times of calls and emails
Step 5: Appeal the Decision (If Necessary)
If the prior authorization request is denied, the healthcare provider can appeal the decision. This involves submitting additional information or documentation to support the request. The healthcare provider should review the denial letter carefully and respond promptly to the appeal.

Conclusion
Obtaining prior authorization for medications like Entyvio can be a complex and time-consuming process. However, by following these 5 essential steps, healthcare providers can simplify the process and ensure that patients receive timely access to necessary treatments. Remember to verify patient eligibility and benefits, gather required documentation, submit the prior authorization request, follow up and respond to additional requests, and appeal the decision if necessary.
Take Action Today!
If you are a healthcare provider or patient seeking prior authorization for Entyvio, take action today by following these 5 essential steps. Don't hesitate to reach out to Aetna or your healthcare provider with any questions or concerns. With persistence and patience, you can navigate the prior authorization process and ensure that patients receive the treatment they need.
What is the purpose of prior authorization?
+Prior authorization is a process used by health insurance companies to determine whether a particular medication or treatment is medically necessary for a patient.
How long does the prior authorization process typically take?
+The prior authorization process can take anywhere from a few days to several weeks, depending on the complexity of the request and the speed of the healthcare provider and insurance company.
Can I appeal a denied prior authorization request?
+Yes, you can appeal a denied prior authorization request. The healthcare provider should review the denial letter carefully and respond promptly to the appeal, submitting additional information or documentation to support the request.