Accolade prior authorization forms are a crucial part of the healthcare process, ensuring that patients receive the necessary medical treatments while minimizing unnecessary costs. However, the complexity of these forms can often lead to frustration and delays. In this article, we will discuss six ways to simplify Accolade prior authorization forms, making the process more efficient for healthcare providers, insurers, and patients alike.
Understanding the Importance of Prior Authorization
Prior authorization is a critical step in the healthcare process, requiring healthcare providers to obtain approval from insurers before administering certain treatments or prescribing specific medications. This process helps prevent unnecessary medical expenses, ensures patient safety, and promotes evidence-based medicine. However, the complexity of prior authorization forms can hinder the efficiency of this process.

Streamlining the Prior Authorization Process
Streamlining the prior authorization process can significantly reduce the administrative burden on healthcare providers, insurers, and patients. By implementing the following strategies, Accolade prior authorization forms can be simplified, making the process more efficient and effective.
1. Electronic Prior Authorization
Electronic prior authorization (ePA) systems can significantly simplify the process by automating the submission and review of prior authorization requests. ePA systems can integrate with existing electronic health records (EHRs) and practice management systems (PMS), reducing manual data entry and minimizing errors. Additionally, ePA systems can provide real-time status updates, reducing the need for phone calls and faxes.

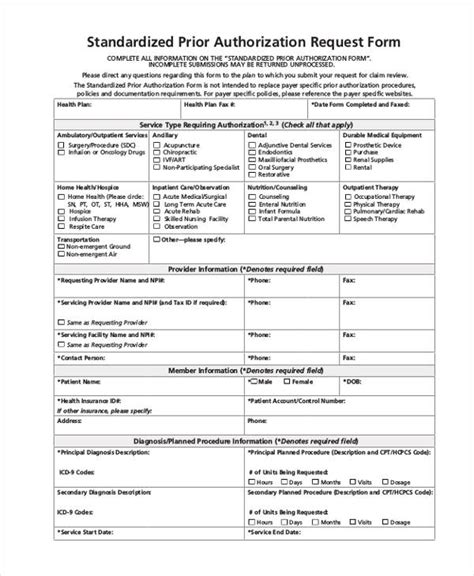
2. Standardized Forms and Templates
Standardized forms and templates can help simplify the prior authorization process by reducing the complexity and variability of the forms. Standardized forms can include clear instructions, pre-populated fields, and easy-to-use interfaces, making it easier for healthcare providers to complete the forms accurately and efficiently.
3. Real-Time Eligibility Verification
Real-time eligibility verification can help streamline the prior authorization process by verifying patient eligibility and benefits in real-time. This can reduce the need for manual verification, minimize errors, and accelerate the prior authorization process.

4. Automated Approval and Denial Notifications
Automated approval and denial notifications can help simplify the prior authorization process by reducing the need for manual communication. Automated notifications can provide timely updates on the status of prior authorization requests, reducing the need for phone calls and faxes.
5. Patient Engagement and Education
Patient engagement and education are critical components of the prior authorization process. By educating patients about the prior authorization process, healthcare providers can empower patients to take a more active role in their care, reducing the likelihood of delays and denials.
6. Data Analytics and Reporting
Data analytics and reporting can help simplify the prior authorization process by providing insights into the efficiency and effectiveness of the process. By analyzing prior authorization data, healthcare providers and insurers can identify areas for improvement, optimize workflows, and reduce costs.

Conclusion: Simplifying Accolade Prior Authorization Forms
Simplifying Accolade prior authorization forms can significantly improve the efficiency and effectiveness of the prior authorization process. By implementing electronic prior authorization, standardized forms and templates, real-time eligibility verification, automated approval and denial notifications, patient engagement and education, and data analytics and reporting, healthcare providers, insurers, and patients can benefit from a streamlined and simplified prior authorization process.

We invite you to share your thoughts on simplifying Accolade prior authorization forms. How have you streamlined the prior authorization process in your organization? Share your experiences and best practices in the comments below.
What is prior authorization?
+Prior authorization is a process that requires healthcare providers to obtain approval from insurers before administering certain treatments or prescribing specific medications.
What are the benefits of electronic prior authorization?
+Electronic prior authorization can automate the submission and review of prior authorization requests, reducing manual data entry and minimizing errors.
How can patient engagement and education improve the prior authorization process?
+Patient engagement and education can empower patients to take a more active role in their care, reducing the likelihood of delays and denials.