The Wellcare Provider Reconsideration Form is an essential document for healthcare providers who want to dispute a denied claim or request a re-evaluation of a payment decision made by Wellcare, a leading health insurance company. Submitting a well-crafted reconsideration form can help providers resolve disputes efficiently and minimize revenue loss. In this article, we will provide a step-by-step guide on how to complete the Wellcare Provider Reconsideration Form and increase the chances of a successful appeal.
Understanding the Reconsideration Process

The reconsideration process is a vital step in resolving disputes between healthcare providers and Wellcare. It allows providers to present additional information, clarify previous submissions, or argue against a denied claim or payment decision. To navigate this process effectively, providers must understand the underlying reasons for the initial denial or payment decision.
Reasons for Reconsideration
Some common reasons for submitting a reconsideration form include:
- Denied claims due to lack of medical necessity or incorrect coding
- Underpayment or overpayment disputes
- Incorrect application of reimbursement policies or rates
- Failure to consider additional information or supporting documentation
Step 1: Gather Required Information

Before starting the reconsideration process, providers must collect all relevant information and documentation, including:
- Patient demographics and medical history
- Claim details, including dates of service and procedure codes
- Reimbursement policies and rates applicable to the claim
- Supporting documentation, such as medical records, test results, and provider notes
- Previous correspondence with Wellcare regarding the claim or payment decision
Organizing Documentation
To ensure a smooth reconsideration process, providers should organize their documentation in a clear and concise manner. This may involve creating a table of contents, indexing supporting documents, and using clear headings and labels.
Step 2: Complete the Reconsideration Form

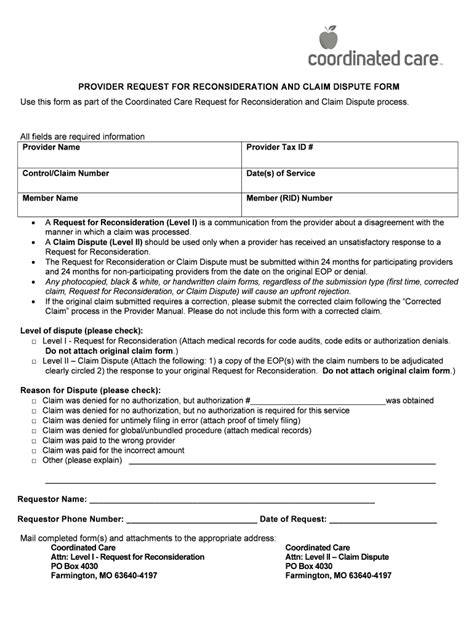
The Wellcare Provider Reconsideration Form typically includes the following sections:
- Claim information, including claim number, patient name, and dates of service
- Reason for reconsideration, with space for detailed explanation and supporting documentation
- Request for reimbursement, including amount and basis for request
- Provider information, including name, address, and contact details
Writing a Clear and Concise Explanation
When completing the reconsideration form, providers should focus on presenting a clear and concise explanation of the reason for reconsideration. This may involve:
- Clearly stating the disputed issue or payment decision
- Providing relevant background information and context
- Outlining the specific grounds for reconsideration, including applicable laws, regulations, or reimbursement policies
- Summarizing supporting documentation and evidence
Step 3: Submit the Reconsideration Form

Once the reconsideration form is complete, providers should submit it to Wellcare via the designated channel, which may include:
- Mail: providers can send the completed form and supporting documentation to Wellcare's reconsideration department
- Fax: providers can fax the completed form and supporting documentation to Wellcare's reconsideration department
- Electronic submission: providers may be able to submit the reconsideration form and supporting documentation electronically through Wellcare's online portal
Tracking and Following Up
After submitting the reconsideration form, providers should track the status of their request and follow up with Wellcare as necessary. This may involve:
- Confirming receipt of the reconsideration form and supporting documentation
- Checking the status of the reconsideration request online or via phone
- Responding to additional requests for information or documentation
Step 4: Respond to Reconsideration Decision

Once Wellcare makes a reconsideration decision, providers should carefully review the outcome and respond accordingly. This may involve:
- Accepting the decision and implementing any necessary changes
- Appealing the decision to the next level of review
- Seeking external review or arbitration
Understanding the Reconsideration Decision
When responding to the reconsideration decision, providers should take the time to understand the underlying reasons for the outcome. This may involve:
- Reviewing the reconsideration decision letter and supporting documentation
- Analyzing the applicable laws, regulations, and reimbursement policies
- Identifying areas for improvement and implementing necessary changes
By following these steps and tips, healthcare providers can increase their chances of a successful appeal and resolve disputes with Wellcare efficiently.
Now it's your turn! Have you ever submitted a Wellcare Provider Reconsideration Form? Share your experiences and tips in the comments below. Don't forget to share this article with your colleagues and friends who may benefit from this information.
What is the purpose of the Wellcare Provider Reconsideration Form?
+The Wellcare Provider Reconsideration Form is used to dispute a denied claim or request a re-evaluation of a payment decision made by Wellcare.
What information is required to complete the reconsideration form?
+Providers must collect all relevant information and documentation, including patient demographics, claim details, reimbursement policies, and supporting documentation.
How do I submit the reconsideration form?
+Providers can submit the reconsideration form and supporting documentation via mail, fax, or electronic submission through Wellcare's online portal.