Prior authorization is a crucial step in the healthcare process, ensuring that patients receive necessary treatments while also controlling costs and promoting evidence-based medicine. For healthcare providers, navigating the prior authorization process can be complex and time-consuming. TurningPoint Healthcare Solutions offers a comprehensive prior authorization form guide to help streamline this process and reduce administrative burdens.
Understanding Prior Authorization

Prior authorization is a process used by healthcare payers to determine whether a particular treatment or service is medically necessary and meets specific criteria. This process aims to ensure that patients receive high-quality, cost-effective care while minimizing unnecessary expenses. However, prior authorization can be a source of frustration for healthcare providers, patients, and payers alike, due to its complexity and variability.
The Role of Prior Authorization in Healthcare
Prior authorization plays a critical role in the healthcare system by:
- Promoting evidence-based medicine
- Reducing unnecessary costs
- Ensuring patient safety
- Improving health outcomes
Despite its importance, prior authorization can be a time-consuming and labor-intensive process, often requiring significant administrative resources.
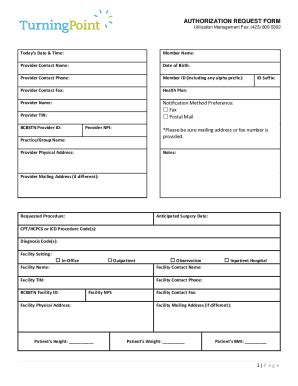
TurningPoint Healthcare Solutions Prior Authorization Form Guide

TurningPoint Healthcare Solutions offers a comprehensive prior authorization form guide to help healthcare providers navigate this complex process. The guide provides a detailed, step-by-step approach to prior authorization, covering topics such as:
- Understanding prior authorization requirements
- Identifying necessary documentation
- Completing prior authorization forms
- Submitting and tracking prior authorization requests
Benefits of Using TurningPoint's Prior Authorization Form Guide
By using TurningPoint's prior authorization form guide, healthcare providers can:
- Reduce administrative burdens
- Improve prior authorization approval rates
- Enhance patient satisfaction
- Increase operational efficiency
Prior Authorization Form Requirements

Prior authorization forms typically require specific information and documentation, including:
- Patient demographics
- Medical history
- Treatment plans
- Supporting documentation (e.g., lab results, medical records)
Healthcare providers must ensure that all necessary information is included and accurate to avoid delays or denials.
Common Prior Authorization Form Mistakes
Common mistakes to avoid when completing prior authorization forms include:
- Incomplete or inaccurate information
- Missing or inadequate documentation
- Failure to follow payer-specific guidelines
- Insufficient medical justification
Prior Authorization Form Submission and Tracking

Once the prior authorization form is complete, healthcare providers must submit it to the payer for review. TurningPoint's prior authorization form guide provides tips on:
- Submitting prior authorization requests electronically or by mail
- Tracking prior authorization status
- Responding to prior authorization requests and denials
Best Practices for Prior Authorization Form Submission and Tracking
Best practices for prior authorization form submission and tracking include:
- Using electronic submission methods whenever possible
- Keeping detailed records of prior authorization requests and responses
- Following up on pending prior authorization requests
Prior Authorization Form Denials and Appeals

Prior authorization denials can be frustrating for healthcare providers and patients. TurningPoint's prior authorization form guide provides guidance on:
- Understanding prior authorization denial reasons
- Appealing prior authorization denials
- Resubmitting prior authorization requests
Common Reasons for Prior Authorization Denials
Common reasons for prior authorization denials include:
- Lack of medical necessity
- Inadequate documentation
- Failure to meet payer-specific guidelines
- Exceeding coverage limits
Conclusion: Streamlining Prior Authorization with TurningPoint's Form Guide

Prior authorization can be a complex and time-consuming process, but with the right tools and guidance, healthcare providers can streamline this process and improve patient outcomes. TurningPoint's prior authorization form guide provides a comprehensive resource for navigating the prior authorization process, reducing administrative burdens, and improving approval rates.
By using TurningPoint's prior authorization form guide, healthcare providers can:
- Improve prior authorization approval rates
- Enhance patient satisfaction
- Increase operational efficiency
- Reduce administrative burdens
We invite you to share your experiences with prior authorization and how you've streamlined this process in your organization. Leave a comment below, and let's continue the conversation!
What is prior authorization?
+Prior authorization is a process used by healthcare payers to determine whether a particular treatment or service is medically necessary and meets specific criteria.
Why is prior authorization important?
+Prior authorization promotes evidence-based medicine, reduces unnecessary costs, ensures patient safety, and improves health outcomes.
What is TurningPoint's prior authorization form guide?
+TurningPoint's prior authorization form guide is a comprehensive resource that provides a step-by-step approach to prior authorization, covering topics such as understanding prior authorization requirements, identifying necessary documentation, completing prior authorization forms, and submitting and tracking prior authorization requests.