Navigating the complexities of Medicare appeals can be a daunting task, especially when dealing with a specific provider like Wellcare. Understanding the process and having a clear guide on how to file a Wellcare Medicare appeal form is crucial for ensuring that your rights as a beneficiary are protected and that you receive the coverage you deserve. This article aims to break down the appeal process into manageable steps, highlighting the key points and providing practical advice on each stage.
Filing a Wellcare Medicare Appeal: Understanding Your Rights

Before diving into the specifics of the appeal process, it's essential to understand your rights as a Medicare beneficiary. The Medicare program is designed to provide health insurance coverage to individuals 65 and older, certain younger people with disabilities, and people with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant). When a claim is denied or partially denied, beneficiaries have the right to appeal the decision.
Why File an Appeal?
Filing an appeal is your opportunity to dispute a decision made by Wellcare or Medicare that you believe is incorrect or unfair. This could be due to a denied claim, a reduction in benefits, or a determination that a service or item is not medically necessary. By appealing, you are asking for a review of the decision, which could potentially result in a reversal or modification of the original determination.
Step 1: Reviewing Your Denial Notice

Upon receiving a denial notice from Wellcare, it's crucial to carefully review the information provided. The notice should include:
- The reason for the denial
- The specific policy or regulation that supports the denial
- Information on how to appeal the decision
- The deadline for filing an appeal
Understanding the reasons behind the denial will help you prepare your appeal by identifying the key points to address.
Key Takeaways:
- Review the denial notice thoroughly
- Understand the reason for the denial
- Note the deadline for appeal
Step 2: Gathering Necessary Documentation

To support your appeal, you'll need to gather relevant documentation. This may include:
- Medical records related to the denied service or item
- Letters from your healthcare provider explaining why the service or item is medically necessary
- Any communication with Wellcare or Medicare related to the claim
- Billing statements and receipts
Having a complete and organized set of documents will strengthen your appeal by providing evidence that supports your claim.
Practical Tips:
- Keep a record of all correspondence with Wellcare and Medicare
- Request a detailed explanation from your healthcare provider
- Ensure all documents are dated and relevant to the appeal
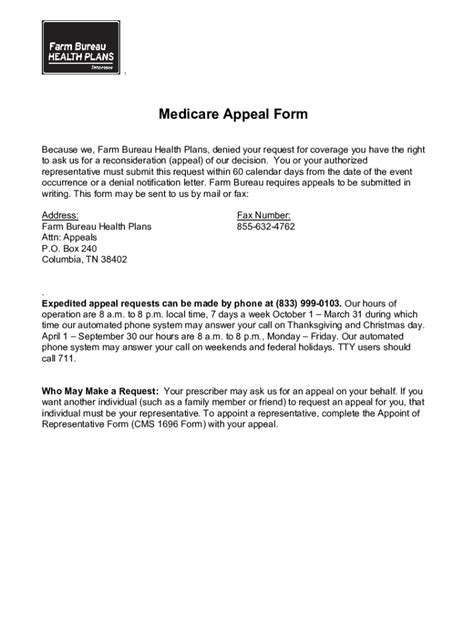
Step 3: Completing the Wellcare Medicare Appeal Form

The appeal form is a critical component of the process. You can usually find the form on Wellcare's website or by contacting their customer service. When completing the form:
- Fill out all required fields accurately
- Attach all supporting documentation
- Clearly state the reason for the appeal and the desired outcome
Ensure you follow the instructions carefully to avoid any delays or complications in the review process.
Best Practices:
- Use a clear and concise writing style
- Attach a cover letter summarizing your appeal
- Keep a copy of the completed form and supporting documents for your records
Step 4: Submitting Your Appeal

Once your appeal form is complete and you have gathered all necessary documentation, it's time to submit your appeal. Ensure you meet the deadline specified in your denial notice to avoid your appeal being dismissed.
Important Considerations:
- Double-check the submission address or fax number
- Use certified mail or a trackable delivery method
- Keep proof of submission
Step 5: Following Up on Your Appeal

After submitting your appeal, it's essential to follow up to ensure it has been received and is being processed. You can contact Wellcare's customer service to inquire about the status of your appeal.
Tips for Effective Follow-Up:
- Keep a record of all follow-up communications
- Be polite but persistent
- Ask for a specific timeline for a decision
Wrapping Up
Filing a Wellcare Medicare appeal form is a significant step in ensuring you receive the coverage you need. By understanding your rights, gathering necessary documentation, completing the appeal form accurately, submitting your appeal on time, and following up on its status, you can navigate the appeal process with confidence.
Take Action Today:
If you've received a denial notice from Wellcare, don't wait. Start the appeal process today to protect your rights and advocate for the coverage you deserve.
How long does a Medicare appeal typically take?
+The length of time a Medicare appeal takes can vary depending on the level of appeal and the complexity of the case. Generally, it can take anywhere from a few weeks to several months to receive a decision.
Can I appeal a Medicare decision more than once?
+Yes, if your initial appeal is denied, you have the right to appeal again, moving through the levels of appeal until you receive a satisfactory decision or reach the final level of appeal.
Do I need to hire a professional to help with my Medicare appeal?
+While it's possible to navigate the appeal process on your own, hiring a professional advocate can provide valuable expertise and support, especially if your case is complex or you are not comfortable representing yourself.