Receiving the right medication at the right time is crucial for effective healthcare. However, navigating the complexities of healthcare systems and insurance coverage can be overwhelming, especially for those who rely on Tricare for their medical needs. One critical aspect of Tricare coverage is the prior authorization process for medications, which ensures that patients receive the necessary medications while controlling costs and ensuring safety. Understanding the Tricare prior authorization form for medication is essential for both healthcare providers and beneficiaries to ensure seamless access to care.
For those who may be unfamiliar, Tricare is a healthcare program sponsored by the US Department of Defense that provides comprehensive coverage to uniformed service members, retirees, and their families. With its various plans, Tricare aims to deliver high-quality care while managing healthcare costs. The prior authorization process is a key component of this cost management strategy, ensuring that prescribed medications are medically necessary and align with established treatment guidelines.
Understanding the Prior Authorization Process for Medication

The prior authorization process involves a series of steps aimed at evaluating the medical necessity of a prescribed medication. Here’s a breakdown of what this process entails:
- Prescription: The process begins with a healthcare provider prescribing a medication that requires prior authorization.
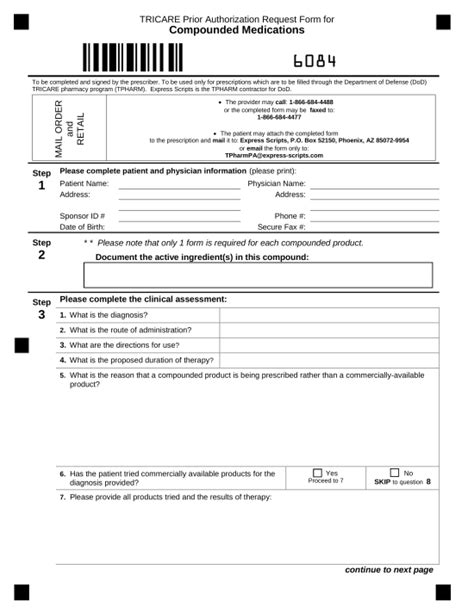
- Submission: The provider or their staff submits a prior authorization request to Tricare, typically through an online portal or by fax/mail, along with supporting documentation.
- Review: Tricare reviews the request, considering factors such as the medication’s effectiveness, potential side effects, and whether it aligns with established treatment guidelines.
- Decision: After review, Tricare makes a determination and notifies the provider. Approvals are typically valid for a specified period, after which the medication may need to be reauthorized.
Key Aspects of the Tricare Prior Authorization Form for Medication
When completing the Tricare prior authorization form for medication, it’s crucial to understand the key aspects that need to be included:
- Patient Information: Accurate patient details, including their Tricare ID number.
- Prescription Information: The name of the medication, dosage, frequency, and duration of treatment.
- Medical Justification: A clear explanation from the healthcare provider detailing the medical necessity of the medication and how it aligns with established treatment guidelines.
- Supporting Documentation: Relevant medical records, test results, or other documentation that supports the prescription.
Benefits of Prior Authorization

While the prior authorization process may seem cumbersome, it offers several benefits:
- Cost Control: Helps manage healthcare costs by ensuring that medications prescribed are medically necessary and cost-effective.
- Safety: Reduces the risk of adverse reactions and interactions by reviewing medications for potential safety issues.
- Quality of Care: Ensures that patients receive high-quality care by adhering to established treatment guidelines.
Challenges and Solutions
Despite its benefits, the prior authorization process can present challenges, including delays in treatment and administrative burdens on healthcare providers. To mitigate these challenges:
- Electronic Prior Authorization: Utilizing electronic prior authorization systems can streamline the process, reducing administrative time and increasing efficiency.
- Clear Communication: Maintaining open and clear communication between healthcare providers, patients, and Tricare is essential for resolving issues promptly and ensuring that patients receive necessary medications without undue delay.
Conclusion and Next Steps

Understanding the Tricare prior authorization form for medication and the underlying process is crucial for both healthcare providers and beneficiaries. By recognizing the importance of prior authorization, its benefits, and how to navigate any challenges, we can work together to ensure that those who rely on Tricare receive the necessary medications without unnecessary delays or complications.
If you have any experiences or questions about the Tricare prior authorization process, we invite you to share them in the comments below. Your insights can help others better understand this critical aspect of healthcare coverage.
What is the purpose of the prior authorization process for medication under Tricare?
+The prior authorization process ensures that prescribed medications are medically necessary, safe, and cost-effective, aligning with established treatment guidelines.
How long does the prior authorization process typically take?
+The processing time can vary but generally takes a few days to a week. However, this timeframe can depend on the complexity of the request and the speed at which necessary information is provided.
Can I appeal if my prior authorization request is denied?
+Yes, if your request is denied, you have the right to appeal. It’s recommended to review the denial reason and work with your healthcare provider to resubmit the request with additional information if necessary.