Gingivitis is a common oral health issue that affects millions of people worldwide. It is the top cause of periodontal disease, a condition that can lead to serious complications if left untreated. Gingivitis is a bacterial infection that causes inflammation of the gums (gingiva) and can eventually lead to the destruction of the tissue that supports the teeth. In this article, we will delve into the world of gingivitis, exploring its causes, symptoms, diagnosis, and treatment options.

Gingivitis is a preventable condition, and good oral hygiene practices can go a long way in preventing its onset. However, despite its preventable nature, gingivitis remains a common problem, especially among adults. According to the Centers for Disease Control and Prevention (CDC), nearly half of all adults in the United States have some form of periodontal disease, with gingivitis being the most common form.
Causes of Gingivitis
Gingivitis is caused by the buildup of plaque, a sticky film of bacteria, on the teeth. Plaque contains toxins that can damage the gums and cause inflammation. If plaque is not removed regularly, it can harden into tartar, which can only be removed by a dental professional. Other factors that can contribute to the development of gingivitis include:
- Poor oral hygiene habits
- Smoking and tobacco use
- Genetics
- Hormonal changes
- Certain medications
- Poor diet

Risk Factors for Gingivitis
While anyone can develop gingivitis, some people are more prone to the condition than others. These include:
- Smokers and tobacco users
- People with a family history of periodontal disease
- Pregnant women
- People with certain medical conditions, such as diabetes and heart disease
- People taking certain medications, such as steroids and certain antidepressants
Symptoms of Gingivitis
Gingivitis can cause a range of symptoms, including:
- Red, swollen, and tender gums
- Bleeding gums, especially when brushing or flossing
- Bad breath (halitosis)
- Loose teeth
- Pain when chewing
- Sensitive teeth

Diagnosing Gingivitis
Gingivitis can be diagnosed by a dental professional during a routine examination. The dentist will examine the gums for signs of inflammation and bleeding, and may also take X-rays to check for any bone loss. A periodontal probe may be used to measure the depth of the gum pockets and check for any signs of gum recession.
Treatment Options for Gingivitis
Gingivitis can be treated with a range of options, including:
- Professional cleaning: A dental professional will remove plaque and tartar from the teeth and below the gum line.
- Scaling and root planing: A deep cleaning procedure that removes plaque and tartar from the teeth and roots.
- Antibiotics: May be prescribed to treat any underlying infections.
- Good oral hygiene practices: Brushing and flossing regularly to prevent the buildup of plaque.

Preventing Gingivitis
Preventing gingivitis is easier than treating it. Good oral hygiene practices can go a long way in preventing the buildup of plaque and tartar. These include:
- Brushing teeth at least twice a day with a fluoride toothpaste
- Flossing once a day to remove plaque and food particles
- Rinsing with mouthwash to kill bacteria
- Visiting a dental professional regularly for check-ups and cleanings
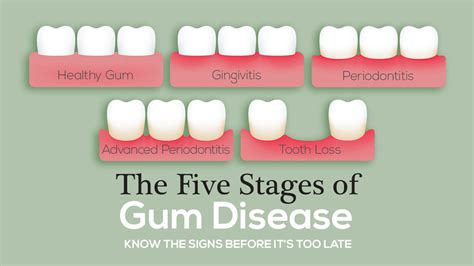
Complications of Untreated Gingivitis
If left untreated, gingivitis can lead to serious complications, including:
- Periodontal disease: A condition that can lead to the loss of teeth and surrounding tissue.
- Heart disease: Research has shown a link between gum disease and an increased risk of heart disease.
- Diabetes: People with gum disease are more likely to develop diabetes.
- Respiratory disease: Bacteria from the mouth can be breathed into the lungs, causing respiratory infections.

In conclusion, gingivitis is a preventable condition that can have serious consequences if left untreated. By practicing good oral hygiene habits and visiting a dental professional regularly, you can prevent gingivitis and maintain good oral health.
What is gingivitis?
+Gingivitis is a bacterial infection that causes inflammation of the gums (gingiva) and can eventually lead to the destruction of the tissue that supports the teeth.
What are the symptoms of gingivitis?
+The symptoms of gingivitis include red, swollen, and tender gums, bleeding gums, bad breath, loose teeth, pain when chewing, and sensitive teeth.
How is gingivitis treated?
+Gingivitis can be treated with professional cleaning, scaling and root planing, antibiotics, and good oral hygiene practices.