Providence prior authorization form is a crucial document for healthcare providers to obtain approval for specific treatments, medications, or services before they can be administered to patients. Prior authorization, also known as pre-authorization or pre-certification, is a process used by insurance companies to determine whether a particular treatment or service is medically necessary and covered under the patient's insurance plan.
The prior authorization process can be complex and time-consuming, requiring significant paperwork and administrative efforts from healthcare providers. However, streamlining the process can help reduce delays, improve patient outcomes, and enhance the overall efficiency of healthcare services. In this article, we will discuss the importance of prior authorization, the benefits of streamlining the process, and provide guidance on how to complete the Providence prior authorization form.
Why is Prior Authorization Important?
Prior authorization is essential in ensuring that patients receive medically necessary treatments while minimizing unnecessary costs and risks. By requiring prior authorization, insurance companies can:
- Ensure that treatments are evidence-based and aligned with established medical guidelines
- Reduce the risk of adverse reactions or complications from unnecessary treatments
- Prevent unnecessary costs and resource utilization
- Improve patient outcomes by ensuring that treatments are tailored to individual needs
Benefits of Streamlining the Prior Authorization Process
Streamlining the prior authorization process can have numerous benefits for healthcare providers, patients, and insurance companies. Some of the advantages include:
- Reduced administrative burdens and paperwork
- Faster approval times and reduced delays in treatment
- Improved patient satisfaction and outcomes
- Enhanced communication and collaboration between healthcare providers and insurance companies
- Reduced costs and resource utilization

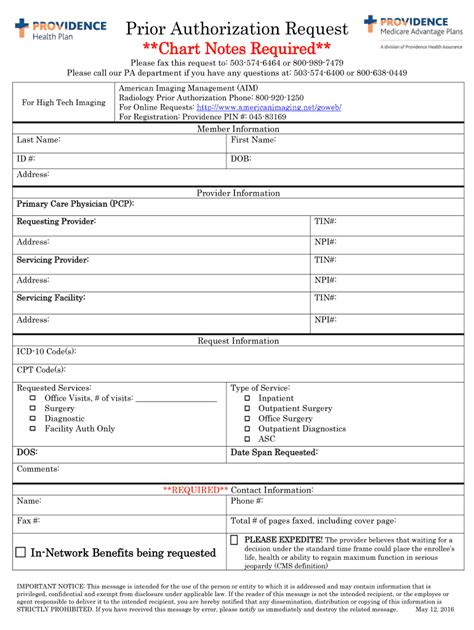
Completing the Providence Prior Authorization Form
To complete the Providence prior authorization form, healthcare providers should follow these steps:
- Gather required information: Ensure that you have all necessary patient information, including demographics, medical history, and treatment plans.
- Choose the correct form: Select the appropriate prior authorization form for the specific treatment or service being requested.
- Complete the form accurately: Fill out the form with accurate and complete information, including patient demographics, treatment plans, and supporting documentation.
- Attach supporting documentation: Include all relevant supporting documentation, such as medical records, test results, and treatment plans.
- Submit the form: Submit the completed form to the insurance company or designated authorized representative.
Tips for Completing the Form
- Use clear and concise language when completing the form
- Ensure that all required fields are completed accurately and thoroughly
- Attach all relevant supporting documentation to avoid delays
- Use a secure and HIPAA-compliant method to submit the form

Common Mistakes to Avoid
When completing the Providence prior authorization form, healthcare providers should avoid the following common mistakes:
- Incomplete or inaccurate information: Ensure that all required fields are completed accurately and thoroughly.
- Missing supporting documentation: Attach all relevant supporting documentation to avoid delays.
- Incorrect form submission: Submit the completed form to the correct insurance company or designated authorized representative.
Best Practices for Streamlining the Prior Authorization Process
- Implement electronic prior authorization: Consider using electronic prior authorization systems to reduce paperwork and administrative burdens.
- Establish clear communication channels: Ensure that healthcare providers and insurance companies have clear communication channels to facilitate the prior authorization process.
- Use standardized forms: Use standardized prior authorization forms to reduce errors and improve efficiency.

By following these tips and best practices, healthcare providers can streamline the prior authorization process, reduce administrative burdens, and improve patient outcomes.
As healthcare providers continue to navigate the complexities of prior authorization, it is essential to prioritize patient-centered care and efficient administrative processes. By working together with insurance companies and adopting streamlined processes, we can ensure that patients receive timely and medically necessary treatments while minimizing unnecessary costs and risks.
We encourage you to share your experiences and insights on streamlining the prior authorization process in the comments below. Your feedback and suggestions can help us improve the efficiency and effectiveness of healthcare services.
What is prior authorization?
+Prior authorization, also known as pre-authorization or pre-certification, is a process used by insurance companies to determine whether a particular treatment or service is medically necessary and covered under the patient's insurance plan.
Why is prior authorization important?
+Prior authorization is essential in ensuring that patients receive medically necessary treatments while minimizing unnecessary costs and risks.
How can I streamline the prior authorization process?
+Streamlining the prior authorization process can be achieved by implementing electronic prior authorization, establishing clear communication channels, and using standardized forms.