The Proact Prior Authorization form is a crucial document that healthcare providers and patients must navigate to ensure that necessary treatments and medications are approved and covered by insurance providers. However, filling out this form can be a daunting task, especially for those who are not familiar with the process. In this article, we will break down the Proact Prior Authorization form into manageable steps, providing you with a clear understanding of what is required and how to simplify the process.
Understanding the Importance of Prior Authorization

Prior authorization is a process that requires healthcare providers to obtain approval from insurance providers before administering certain treatments or prescribing specific medications. This process is in place to ensure that patients receive necessary and effective care while minimizing unnecessary costs. By understanding the importance of prior authorization, you can better navigate the Proact Prior Authorization form and ensure that your patients receive the care they need.
Step 1: Gather Required Information

The first step in simplifying the Proact Prior Authorization form is to gather all the required information. This includes:
- Patient demographics and contact information
- Medical history and diagnosis
- Treatment plan and medication list
- Insurance provider information and policy details
Having all the necessary information readily available will help you to complete the form accurately and efficiently.
Required Documents
- Patient's medical records
- Insurance provider's policy documents
- Treatment plan and medication list
Step 2: Determine the Type of Prior Authorization

There are two types of prior authorization:
- Standard prior authorization: This type of authorization is required for non-emergency treatments and medications.
- Expedited prior authorization: This type of authorization is required for emergency treatments and medications.
Determine the type of prior authorization required and complete the form accordingly.
Prior Authorization Types
- Standard prior authorization
- Expedited prior authorization
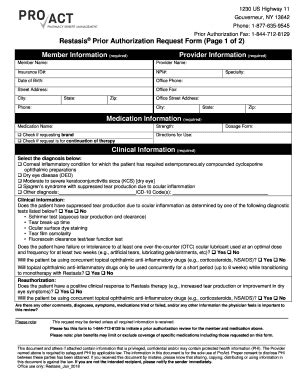
Step 3: Complete the Proact Prior Authorization Form

Once you have gathered all the required information and determined the type of prior authorization, you can complete the Proact Prior Authorization form. Make sure to:
- Fill out the form accurately and completely
- Include all required documents and information
- Sign and date the form
Proact Prior Authorization Form Requirements
- Patient demographics and contact information
- Medical history and diagnosis
- Treatment plan and medication list
- Insurance provider information and policy details
Step 4: Submit the Form and Supporting Documents

Once the form is complete, submit it to the insurance provider along with all supporting documents. Make sure to:
- Submit the form and documents via the required method (e.g. fax, email, or mail)
- Keep a copy of the submitted form and documents for your records
Submission Methods
- Fax
Step 5: Follow Up and Track the Status

After submitting the form and supporting documents, follow up with the insurance provider to track the status of the prior authorization. Make sure to:
- Contact the insurance provider via phone or email to inquire about the status
- Keep a record of all communication and correspondence
Tracking Status
- Contact insurance provider via phone or email
- Keep record of all communication and correspondence
By following these 5 steps, you can simplify the Proact Prior Authorization form and ensure that your patients receive the necessary care and treatment.
We invite you to share your experiences and tips for navigating the Proact Prior Authorization form in the comments section below. Your feedback and insights can help others to better understand and simplify the process.
What is prior authorization?
+Prior authorization is a process that requires healthcare providers to obtain approval from insurance providers before administering certain treatments or prescribing specific medications.
What is the Proact Prior Authorization form?
+The Proact Prior Authorization form is a document that healthcare providers must complete to request prior authorization from insurance providers.
How long does the prior authorization process take?
+The prior authorization process can take several days to several weeks, depending on the insurance provider and the type of authorization required.