The prior authorization process can be a daunting task for healthcare providers, especially when dealing with complex forms and tedious paperwork. The Navinet prior authorization form is one such document that can seem overwhelming at first glance. However, with a clear understanding of its components and a simplified explanation, healthcare providers can navigate this process with ease.
Prior authorization is a critical step in ensuring that patients receive the necessary medical treatments and prescriptions while also controlling healthcare costs. The Navinet prior authorization form is designed to streamline this process, making it more efficient for healthcare providers to obtain approval for their patients' treatments.
What is the Navinet Prior Authorization Form?

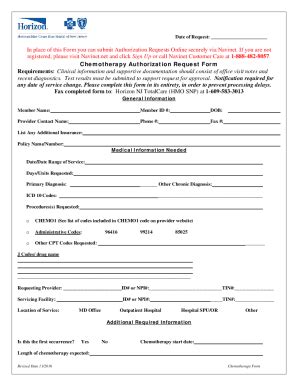
The Navinet prior authorization form is a document used by healthcare providers to request prior authorization for medical treatments, procedures, and prescriptions. This form is typically used by healthcare providers who are part of the Navinet network, which includes a wide range of healthcare organizations and payers.
The form is designed to gather all the necessary information required for prior authorization, including patient demographics, treatment plans, and medical histories. By providing this information, healthcare providers can ensure that their patients receive the necessary approvals for their treatments in a timely and efficient manner.
Components of the Navinet Prior Authorization Form
The Navinet prior authorization form typically includes several components, including:
- Patient demographics: This section includes information about the patient, such as name, date of birth, and contact information.
- Treatment plan: This section outlines the proposed treatment plan, including the type of treatment, dosage, and frequency.
- Medical history: This section includes information about the patient's medical history, including any previous treatments, allergies, and medical conditions.
- Clinical rationale: This section provides a clear explanation of why the proposed treatment is necessary and how it will benefit the patient.
- Supporting documentation: This section includes any supporting documentation, such as medical records, test results, and prescriptions.
How to Complete the Navinet Prior Authorization Form

Completing the Navinet prior authorization form can seem like a daunting task, but by following these steps, healthcare providers can ensure that the form is filled out accurately and efficiently.
- Gather all necessary information: Before starting the form, gather all the necessary information, including patient demographics, treatment plans, and medical histories.
- Fill out the patient demographics section: Complete this section accurately, ensuring that all information is up-to-date and correct.
- Outline the treatment plan: Clearly outline the proposed treatment plan, including the type of treatment, dosage, and frequency.
- Provide medical history: Include any relevant medical history, including previous treatments, allergies, and medical conditions.
- Provide clinical rationale: Clearly explain why the proposed treatment is necessary and how it will benefit the patient.
- Attach supporting documentation: Include any supporting documentation, such as medical records, test results, and prescriptions.
- Review and submit: Review the form carefully before submitting it to ensure that all information is accurate and complete.
Tips for Streamlining the Prior Authorization Process
- Use electronic prior authorization systems: Electronic prior authorization systems can streamline the process, reducing paperwork and increasing efficiency.
- Ensure accurate and complete information: Ensure that all information is accurate and complete, reducing the risk of delays or denials.
- Use clear and concise language: Use clear and concise language when completing the form, ensuring that all information is easy to understand.
- Attach supporting documentation: Attach any supporting documentation, such as medical records and test results, to ensure that the form is complete.
Benefits of Using the Navinet Prior Authorization Form

The Navinet prior authorization form offers several benefits to healthcare providers, including:
- Streamlined prior authorization process: The form is designed to streamline the prior authorization process, reducing paperwork and increasing efficiency.
- Improved accuracy: The form ensures that all necessary information is gathered, reducing the risk of errors or delays.
- Faster approvals: The form is designed to provide all the necessary information required for prior authorization, reducing the risk of delays or denials.
- Enhanced patient care: The form ensures that patients receive the necessary treatments and prescriptions in a timely and efficient manner.
Common Challenges with the Navinet Prior Authorization Form
- Completing the form accurately: The form can be complex and time-consuming to complete, especially for healthcare providers who are new to the prior authorization process.
- Gathering supporting documentation: Gathering supporting documentation can be time-consuming, especially for healthcare providers who have limited resources.
- Dealing with denials: Dealing with denials can be frustrating, especially for healthcare providers who have invested time and resources into completing the form.
Conclusion
The Navinet prior authorization form is a critical document that healthcare providers use to request prior authorization for medical treatments, procedures, and prescriptions. By understanding the components of the form and following the steps outlined in this article, healthcare providers can navigate the prior authorization process with ease. The form offers several benefits, including a streamlined prior authorization process, improved accuracy, and faster approvals. However, healthcare providers may face challenges when completing the form, including gathering supporting documentation and dealing with denials.
We invite you to share your experiences with the Navinet prior authorization form in the comments section below. How do you navigate the prior authorization process? What challenges have you faced, and how have you overcome them? Share your thoughts and insights with us, and let's start a conversation about streamlining the prior authorization process.
What is the purpose of the Navinet prior authorization form?
+The Navinet prior authorization form is used by healthcare providers to request prior authorization for medical treatments, procedures, and prescriptions.
How do I complete the Navinet prior authorization form?
+Completing the Navinet prior authorization form involves gathering all necessary information, including patient demographics, treatment plans, and medical histories. The form should be filled out accurately and completely, with all supporting documentation attached.
What are the benefits of using the Navinet prior authorization form?
+The Navinet prior authorization form offers several benefits, including a streamlined prior authorization process, improved accuracy, and faster approvals.