Molina Medicaid prior authorization (prior auth) forms are an essential part of the healthcare process for patients covered by Molina Medicaid. Prior authorization is a requirement for certain medical treatments, procedures, and medications to ensure that they are medically necessary and cost-effective. In this article, we will guide you through the process of completing a Molina Medicaid prior auth form, explain the importance of prior authorization, and provide valuable insights into the benefits of this process.
What is Prior Authorization?
Prior authorization is a process used by health insurance companies, including Molina Medicaid, to determine whether a specific medical treatment, procedure, or medication is medically necessary and cost-effective. This process involves reviewing a patient's medical history, current health condition, and treatment options to ensure that the proposed treatment is the most appropriate and effective choice.
Why is Prior Authorization Important?
Prior authorization is important for several reasons:
- Ensures medically necessary treatment: Prior authorization helps ensure that patients receive treatment that is medically necessary and aligns with evidence-based medicine.
- Reduces healthcare costs: By reviewing treatment options and ensuring that patients receive the most cost-effective treatment, prior authorization helps reduce healthcare costs.
- Improves patient outcomes: Prior authorization helps improve patient outcomes by ensuring that patients receive the most effective treatment for their specific condition.
How to Complete a Molina Medicaid Prior Auth Form
Completing a Molina Medicaid prior auth form can seem daunting, but it's a straightforward process. Here's a step-by-step guide to help you complete the form:
- Gather required information: Before starting the prior auth form, gather all required information, including the patient's medical history, current health condition, and treatment options.
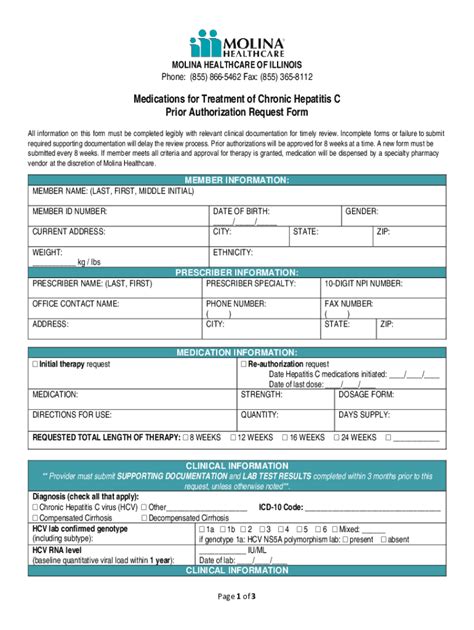
- Choose the correct form: Ensure you have the correct prior auth form for the specific treatment or medication you are requesting.
- Fill out patient information: Complete the patient's demographic information, including name, date of birth, and Medicaid ID number.
- Provide medical information: Provide detailed medical information, including the patient's current health condition, medical history, and treatment options.
- Specify treatment or medication: Clearly specify the treatment or medication you are requesting prior authorization for.
- Provide supporting documentation: Attach supporting documentation, such as medical records, test results, and physician statements, to support the prior auth request.
- Submit the form: Submit the completed prior auth form to Molina Medicaid for review.

Molina Medicaid Prior Auth Form Requirements
To ensure a smooth prior auth process, Molina Medicaid requires the following:
- Complete and accurate information: Ensure all information on the prior auth form is complete and accurate.
- Supporting documentation: Attach supporting documentation to support the prior auth request.
- Timely submission: Submit the prior auth form in a timely manner to avoid delays in treatment.
Benefits of Prior Authorization
Prior authorization offers several benefits, including:
- Improved patient outcomes: Prior authorization helps ensure patients receive the most effective treatment for their specific condition.
- Reduced healthcare costs: Prior authorization helps reduce healthcare costs by ensuring patients receive cost-effective treatment.
- Streamlined treatment process: Prior authorization streamlines the treatment process by ensuring that patients receive the necessary treatment in a timely manner.
Common Mistakes to Avoid
When completing a Molina Medicaid prior auth form, avoid the following common mistakes:
- Incomplete information: Ensure all information on the prior auth form is complete and accurate.
- Lack of supporting documentation: Attach supporting documentation to support the prior auth request.
- Timely submission: Submit the prior auth form in a timely manner to avoid delays in treatment.

Conclusion
Molina Medicaid prior auth forms are an essential part of the healthcare process. By understanding the importance of prior authorization and following the steps outlined in this guide, you can ensure a smooth prior auth process and provide the best possible care for your patients. Remember to avoid common mistakes and take advantage of the benefits of prior authorization to improve patient outcomes and reduce healthcare costs.
Additional Tips
- Check Molina Medicaid's website: Check Molina Medicaid's website for the most up-to-date prior auth forms and requirements.
- Contact Molina Medicaid: Contact Molina Medicaid's customer service department if you have any questions or concerns about the prior auth process.
- Seek professional help: Seek professional help if you need assistance completing the prior auth form.
We hope this guide has been helpful in understanding the Molina Medicaid prior auth form process. If you have any further questions or concerns, please don't hesitate to reach out.
FAQ Section
What is prior authorization?
+Prior authorization is a process used by health insurance companies to determine whether a specific medical treatment, procedure, or medication is medically necessary and cost-effective.
Why is prior authorization important?
+Prior authorization ensures medically necessary treatment, reduces healthcare costs, and improves patient outcomes.
How do I complete a Molina Medicaid prior auth form?
+Follow the steps outlined in this guide to complete a Molina Medicaid prior auth form.