In today's healthcare landscape, managing prior authorizations can be a daunting task for healthcare providers. The Molina Marketplace, a popular health insurance platform, requires providers to navigate its specific prior auth requirements to ensure smooth patient care. To help you optimize your workflow and minimize delays, we've compiled five essential tips to streamline your Molina Marketplace experience.
Understanding Prior Authorizations on the Molina Marketplace

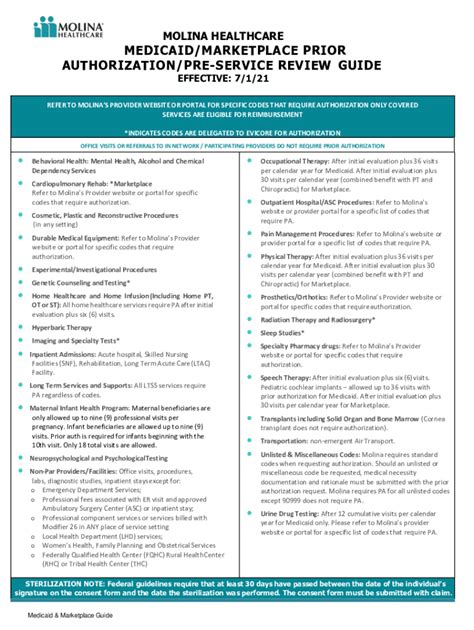
Prior authorizations are a crucial step in ensuring that patients receive necessary medical treatments while preventing unnecessary costs. On the Molina Marketplace, prior auths are required for various services, including prescription medications, medical procedures, and durable medical equipment. By understanding the prior auth process, you can proactively manage your workflow and reduce administrative burdens.
Prior Auth Requirements on the Molina Marketplace
Before diving into our top tips, it's essential to understand the prior auth requirements on the Molina Marketplace. These requirements may vary depending on the specific insurance plan and service being requested. Generally, prior auths are required for:
- High-cost or specialty medications
- Medical procedures, such as surgeries or imaging tests
- Durable medical equipment, like wheelchairs or oxygen therapy
- Behavioral health services, including therapy sessions or counseling
Tips to Streamline Your Molina Marketplace Experience

Now that you understand the prior auth requirements on the Molina Marketplace, it's time to optimize your workflow. Here are our top five tips to help you streamline your experience:
1. Verify Patient Eligibility and Benefits
Verifying patient eligibility and benefits is the first step in ensuring a smooth prior auth process. Use the Molina Marketplace portal or contact their customer service to confirm the patient's coverage and any applicable prior auth requirements. This step helps prevent unnecessary delays and reduces the risk of denied claims.
2. Gather Required Documentation and Information
When submitting a prior auth request, make sure you have all required documentation and information readily available. This may include:
- Patient medical records, including diagnosis and treatment plans
- Prescription information, including medication names and dosages
- Detailed descriptions of medical procedures or services
- Supporting documentation, such as lab results or medical imaging reports
3. Use the Molina Marketplace Portal for Efficient Submission
The Molina Marketplace portal offers a convenient and efficient way to submit prior auth requests. By using the portal, you can:
- Electronically submit prior auth requests, reducing paperwork and administrative burdens
- Track the status of your requests in real-time
- Receive notifications and updates on prior auth decisions
4. Stay Up-to-Date with Molina Marketplace Prior Auth Policies
Molina Marketplace prior auth policies and requirements can change frequently. Stay informed by regularly reviewing the Molina Marketplace website, attending webinars, or participating in training sessions. This helps ensure you're aware of any updates or changes that may impact your prior auth workflow.
5. Leverage Molina Marketplace Resources and Support
The Molina Marketplace offers various resources and support options to help you navigate the prior auth process. Take advantage of these resources, including:
- Customer service: Contact Molina Marketplace customer service for assistance with prior auth requests or to address any questions or concerns.
- Provider manuals: Review the Molina Marketplace provider manual for detailed information on prior auth requirements and procedures.
- Webinars and training sessions: Participate in webinars and training sessions to stay up-to-date on Molina Marketplace policies and procedures.
Maximizing Efficiency with Prior Auth Automation

While the tips above can help streamline your Molina Marketplace experience, automating prior auths can take your efficiency to the next level. Prior auth automation solutions can help you:
- Electronically submit prior auth requests, reducing administrative burdens
- Track prior auth status in real-time, minimizing delays
- Receive notifications and updates on prior auth decisions, ensuring timely patient care
Benefits of Prior Auth Automation
Prior auth automation offers numerous benefits, including:
- Reduced administrative burdens: Automation simplifies the prior auth process, freeing up staff to focus on patient care.
- Improved efficiency: Automated prior auths reduce delays and minimize the risk of denied claims.
- Enhanced patient satisfaction: Timely prior auths ensure patients receive necessary medical treatments without unnecessary delays.
Conclusion: Streamlining Your Molina Marketplace Experience

By implementing these five tips and leveraging prior auth automation solutions, you can significantly streamline your Molina Marketplace experience. Remember to stay informed about Molina Marketplace policies and procedures, and don't hesitate to reach out to their customer service team for support. With these strategies in place, you'll be better equipped to manage prior auths, reduce administrative burdens, and provide timely patient care.
We encourage you to share your experiences with the Molina Marketplace and prior auth automation in the comments below. Your insights can help others optimize their workflows and improve patient outcomes.
What is the Molina Marketplace prior auth process?
+The Molina Marketplace prior auth process involves verifying patient eligibility and benefits, gathering required documentation and information, submitting prior auth requests, and tracking the status of these requests.
How can I check the status of my prior auth requests on the Molina Marketplace?
+You can check the status of your prior auth requests on the Molina Marketplace portal or by contacting their customer service team.
What are the benefits of automating prior auths on the Molina Marketplace?
+Prior auth automation on the Molina Marketplace can reduce administrative burdens, improve efficiency, and enhance patient satisfaction.