Completing a Molina authorization form is a crucial step in ensuring that patients receive the medical treatment they need. As a healthcare provider, it's essential to understand the importance of accurate and timely completion of these forms to avoid delays or denials of treatment. In this article, we will explore five ways to complete a Molina authorization form, providing you with the necessary guidance to streamline the process.
Understanding the Importance of Molina Authorization Forms

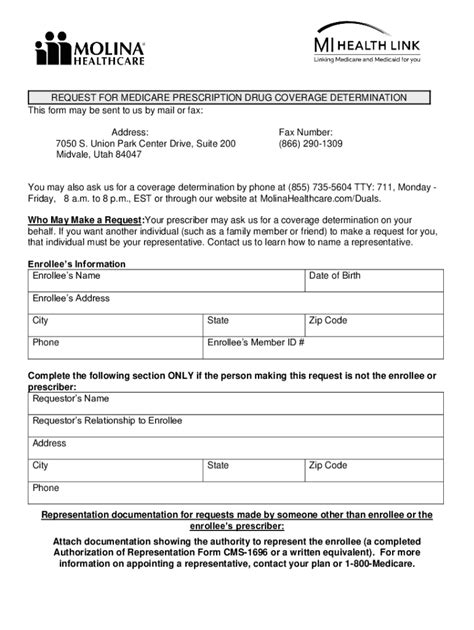
Molina authorization forms are used by healthcare providers to request prior authorization for medical services, treatments, or medications. These forms are typically required by insurance companies, including Molina Healthcare, to ensure that patients receive necessary and covered services. Accurate completion of these forms is critical to avoid delays or denials of treatment, which can have serious consequences for patients.
Why Is It Essential to Complete Molina Authorization Forms Correctly?
Completing Molina authorization forms correctly is essential for several reasons:
- Ensures timely access to necessary medical treatment
- Reduces the risk of delayed or denied treatment
- Helps to prevent costly and time-consuming appeals processes
- Enhances patient satisfaction and outcomes
- Supports compliance with regulatory requirements
5 Ways to Complete a Molina Authorization Form
1. Gather Required Information
Before starting the authorization form, gather all required information, including:
- Patient demographics and insurance details
- Medical records and treatment history
- Prescribing physician's information
- Treatment or service details
What Information Is Typically Required on a Molina Authorization Form?
- Patient's name, date of birth, and insurance ID number
- Diagnosis and treatment codes (ICD-10 and CPT)
- Prescribing physician's name, address, and NPI number
- Treatment or service details, including dates and locations
2. Use the Correct Form
Ensure you are using the most up-to-date and correct Molina authorization form for the specific service or treatment being requested.
How to Obtain the Correct Molina Authorization Form?
- Visit the Molina Healthcare website and navigate to the "Providers" section
- Contact Molina's customer service department for assistance
- Use a secure online portal or electronic health record (EHR) system to access and complete the form
3. Complete the Form Accurately and Thoroughly
Complete the authorization form accurately and thoroughly, ensuring all required fields are filled in correctly.
Tips for Completing the Molina Authorization Form Accurately:
- Use a legible font and avoid abbreviations
- Ensure all required fields are completed
- Double-check patient demographics and insurance details
- Attach supporting medical records and documentation as required
4. Submit the Form in a Timely Manner
Submit the completed authorization form in a timely manner to avoid delays in treatment.
What Are the Typical Submission Deadlines for Molina Authorization Forms?
- Check with Molina Healthcare for specific submission deadlines
- Submit the form at least 7-10 days prior to the scheduled treatment or service
5. Follow Up on the Status of the Authorization
Follow up on the status of the authorization to ensure it has been processed and approved.
How to Follow Up on the Status of a Molina Authorization?
- Contact Molina's customer service department for assistance
- Use a secure online portal or EHR system to track the status of the authorization
- Follow up with the patient to ensure they are aware of the status of their treatment
Conclusion: Streamlining the Molina Authorization Process
Completing a Molina authorization form is a critical step in ensuring patients receive the medical treatment they need. By following these five ways to complete a Molina authorization form, healthcare providers can streamline the process, reduce errors, and improve patient outcomes.
Share Your Thoughts!
Have you experienced challenges with completing Molina authorization forms? Share your thoughts and experiences in the comments below. Your feedback can help us improve our content and provide better guidance for healthcare providers.
Take Action!
- Bookmark this article for future reference
- Share this article with your colleagues and peers
- Contact Molina Healthcare for more information on their authorization process
What is a Molina authorization form?
+A Molina authorization form is a document used by healthcare providers to request prior authorization for medical services, treatments, or medications from Molina Healthcare.
Why is it essential to complete Molina authorization forms correctly?
+Completing Molina authorization forms correctly is essential to ensure timely access to necessary medical treatment, reduce the risk of delayed or denied treatment, and enhance patient satisfaction and outcomes.
How do I obtain the correct Molina authorization form?
+You can obtain the correct Molina authorization form by visiting the Molina Healthcare website, contacting their customer service department, or using a secure online portal or electronic health record (EHR) system.