The Molina appeals form is a crucial document for individuals who receive healthcare services through Molina Healthcare, a prominent health insurance provider in the United States. If you're a Molina member and disagree with a decision made by the company, you have the right to appeal. In this article, we'll delve into the world of Molina appeals, providing a comprehensive guide on how to navigate the process.
Navigating the complexities of healthcare can be overwhelming, especially when dealing with denied claims or services. That's why understanding the appeals process is vital for Molina members. By knowing your rights and the steps involved, you can effectively advocate for yourself and ensure you receive the necessary care. In the following sections, we'll break down the Molina appeals form and provide a step-by-step guide on how to complete it.

Understanding the Molina Appeals Process
Before we dive into the step-by-step guide, it's essential to understand the basics of the Molina appeals process. Molina Healthcare has a dedicated department for handling appeals, ensuring that all decisions are reviewed and reconsidered. The appeals process typically involves the following stages:
- Initial Review: Molina's initial review of your claim or service request.
- First-Level Appeal: If your claim is denied, you can submit a first-level appeal to Molina's appeals department.
- Second-Level Appeal: If your first-level appeal is denied, you can submit a second-level appeal to an independent review organization (IRO).
- External Review: If your second-level appeal is denied, you can request an external review by an independent review organization (IRO).

Step 1: Gathering Required Information
Before you start filling out the Molina appeals form, make sure you have the following information readily available:
- Your Molina member ID number
- The date of the service or claim in question
- A detailed description of the issue or concern
- Supporting documentation, such as medical records or bills
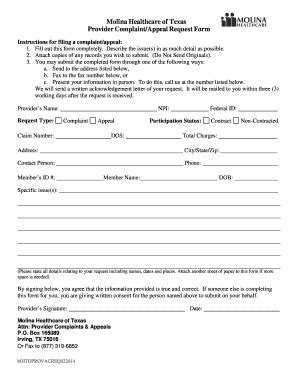
Completing the Molina Appeals Form
Now that you have the necessary information, let's move on to completing the Molina appeals form. The form typically consists of several sections, which we'll outline below:

Section 1: Member Information
In this section, you'll need to provide your personal and plan information, including:
- Your name and Molina member ID number
- Your plan type and effective date
- Your contact information, including address and phone number
Section 2: Appeal Information
In this section, you'll need to provide details about the appeal, including:
- The date of the service or claim in question
- A detailed description of the issue or concern
- The reason for the appeal
Section 3: Supporting Documentation
In this section, you'll need to attach supporting documentation, such as:
- Medical records or bills
- Letters from healthcare providers
- Other relevant documents
Submitting the Molina Appeals Form
Once you've completed the Molina appeals form, you can submit it to the company via mail, fax, or email. Make sure to follow the submission instructions carefully to ensure your appeal is processed promptly.

What to Expect After Submitting the Appeal
After submitting the Molina appeals form, you can expect the following:
- Acknowledgement: Molina will send you an acknowledgement letter confirming receipt of your appeal.
- Review: Molina's appeals department will review your appeal and make a decision.
- Decision: You'll receive a decision letter outlining the outcome of your appeal.
Additional Tips and Reminders
When navigating the Molina appeals process, keep the following tips and reminders in mind:
- Stay organized: Keep all your documents and records organized, including your Molina member ID number and claim information.
- Be patient: The appeals process can take time, so be patient and don't hesitate to reach out to Molina if you have questions or concerns.
- Seek help: If you're having trouble navigating the appeals process, don't hesitate to seek help from a patient advocate or healthcare professional.

Conclusion
The Molina appeals form is a crucial document for individuals who receive healthcare services through Molina Healthcare. By understanding the appeals process and following the step-by-step guide outlined in this article, you can effectively navigate the system and advocate for yourself. Remember to stay organized, be patient, and seek help when needed. If you have any further questions or concerns, don't hesitate to reach out to Molina or a patient advocate.

We hope this article has provided you with valuable insights and information on the Molina appeals process. If you have any feedback or suggestions, please let us know in the comments below. Don't forget to share this article with others who may find it helpful.
What is the Molina appeals process?
+The Molina appeals process is a series of steps that allow Molina members to dispute decisions made by the company. The process typically involves an initial review, first-level appeal, second-level appeal, and external review.
How do I complete the Molina appeals form?
+To complete the Molina appeals form, you'll need to provide your member information, appeal information, and supporting documentation. You can submit the form via mail, fax, or email.
What happens after I submit the Molina appeals form?
+After submitting the Molina appeals form, you can expect to receive an acknowledgement letter, followed by a review of your appeal. You'll receive a decision letter outlining the outcome of your appeal.