Managing healthcare benefits can be a complex process, especially when it comes to ensuring that employees receive the necessary medical treatments. One crucial aspect of this process is the prior authorization form, which helps to determine the necessity and coverage of certain medical procedures. For companies using Meritain Health, a leading provider of employee health benefits, understanding the Meritain Prior Authorization Form is essential. In this article, we will break down the process into 5 easy steps to help you navigate this often-confusing aspect of healthcare management.

Step 1: Understanding Prior Authorization
Prior authorization, also known as pre-certification or pre-authorization, is a process used by health insurance companies to determine whether a particular medical treatment or service is medically necessary and covered under the patient's health plan. This process is designed to ensure that patients receive necessary care while also controlling healthcare costs. For Meritain Health plan holders, understanding what services require prior authorization is crucial for avoiding unexpected medical bills.
Why is Prior Authorization Important?
Prior authorization is important for several reasons:
- It helps to ensure that patients receive medically necessary treatments.
- It reduces the risk of unexpected medical bills.
- It helps to control healthcare costs by preventing unnecessary treatments.
- It ensures that patients are aware of the coverage and costs associated with their medical care.
Step 2: Identifying Services Requiring Prior Authorization
Not all medical services require prior authorization. However, certain treatments and procedures may need pre-approval before they can be covered under a Meritain Health plan. Some examples of services that may require prior authorization include:
- Hospital stays
- Outpatient surgeries
- High-cost medications
- Certain medical equipment
- Mental health services
It's essential to check with Meritain Health to determine which services require prior authorization.
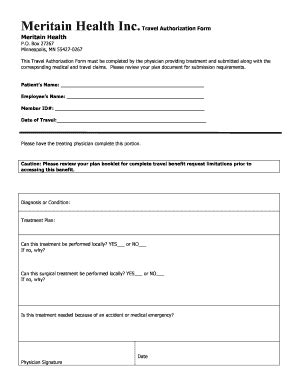
Step 3: Gathering Required Information
To complete the Meritain Prior Authorization Form, you will need to gather certain information. This may include:
- Patient demographics (name, date of birth, etc.)
- Policy information (policy number, etc.)
- Medical information (diagnosis, treatment plan, etc.)
- Supporting documentation (medical records, test results, etc.)
Having this information readily available will help to streamline the prior authorization process.

Step 4: Completing the Meritain Prior Authorization Form
Once you have gathered the required information, you can complete the Meritain Prior Authorization Form. This form can usually be found on the Meritain Health website or by contacting their customer service department. Be sure to fill out the form accurately and thoroughly, as incomplete or inaccurate information may delay the prior authorization process.
Tips for Completing the Form:
- Read the form carefully and follow the instructions.
- Fill out the form accurately and thoroughly.
- Attach all required supporting documentation.
- Submit the form in a timely manner to avoid delays.
Step 5: Submitting the Form and Receiving a Decision
Once you have completed the Meritain Prior Authorization Form, submit it to Meritain Health for review. The review process typically takes a few days to a few weeks, depending on the complexity of the request. After reviewing the form and supporting documentation, Meritain Health will make a determination regarding coverage.
If your request is approved, you will receive a notification indicating the covered services and any applicable costs. If your request is denied, you will receive a notification explaining the reasons for the denial and any appeal options.

By following these 5 easy steps, you can navigate the Meritain Prior Authorization Form process with confidence. Remember to carefully review the form requirements, gather all necessary information, and submit the form in a timely manner to avoid delays. If you have any questions or concerns, don't hesitate to reach out to Meritain Health for assistance.
We hope this guide has been helpful in explaining the Meritain Prior Authorization Form process. If you have any further questions or would like to share your experiences with prior authorization, please leave a comment below. Share this article with others who may find it helpful, and don't forget to subscribe to our blog for more informative articles on healthcare and employee benefits.
What is prior authorization?
+Prior authorization, also known as pre-certification or pre-authorization, is a process used by health insurance companies to determine whether a particular medical treatment or service is medically necessary and covered under the patient's health plan.
Why is prior authorization important?
+Prior authorization is important because it helps to ensure that patients receive medically necessary treatments, reduces the risk of unexpected medical bills, controls healthcare costs, and ensures that patients are aware of the coverage and costs associated with their medical care.
What services require prior authorization?
+Not all medical services require prior authorization. However, certain treatments and procedures may need pre-approval before they can be covered under a Meritain Health plan. Examples of services that may require prior authorization include hospital stays, outpatient surgeries, high-cost medications, certain medical equipment, and mental health services.