The prior authorization process for prescription medications can be a daunting task for many healthcare providers and patients. The Carelon Rx Prior Authorization Form is a crucial document that streamlines this process, ensuring that patients receive the necessary medications while also controlling healthcare costs. In this article, we will provide an easy guide to understanding and completing the Carelon Rx Prior Authorization Form, as well as information on how to download the form.

What is Prior Authorization?
Prior authorization is a process used by health insurance companies to determine whether a particular medication or treatment is medically necessary and covered under the patient's insurance plan. This process helps to control healthcare costs by ensuring that patients receive only necessary and cost-effective treatments. Prior authorization is usually required for medications that are expensive, have potential side effects, or have alternative treatments available.
Why is Prior Authorization Important?
Prior authorization is essential for several reasons:
- It ensures that patients receive medically necessary treatments that are covered under their insurance plan.
- It helps to control healthcare costs by reducing unnecessary or duplicate treatments.
- It promotes safe and effective use of medications by ensuring that patients are not over-medicated or under-medicated.
- It enables healthcare providers to provide high-quality care while minimizing costs.
What is the Carelon Rx Prior Authorization Form?
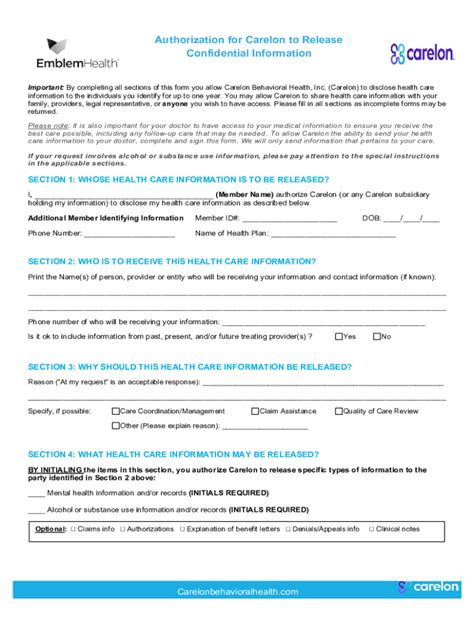
The Carelon Rx Prior Authorization Form is a document used by healthcare providers to request prior authorization for prescription medications. The form is designed to gather necessary information about the patient's medical condition, the prescribed medication, and the treatment plan. The form is then submitted to Carelon Rx, a pharmacy benefit management company, for review and approval.

How to Complete the Carelon Rx Prior Authorization Form
Completing the Carelon Rx Prior Authorization Form requires careful attention to detail and accurate information. Here's a step-by-step guide to help you complete the form:
- Patient Information: Enter the patient's name, date of birth, and insurance identification number.
- Prescriber Information: Enter the healthcare provider's name, contact information, and National Provider Identifier (NPI) number.
- Medication Information: Enter the name of the prescribed medication, dosage, frequency, and duration of treatment.
- Medical Condition: Describe the patient's medical condition and the rationale for prescribing the medication.
- Treatment Plan: Outline the treatment plan, including any alternative treatments or medications that have been tried.
Downloading the Carelon Rx Prior Authorization Form
The Carelon Rx Prior Authorization Form can be downloaded from the Carelon Rx website or by contacting their customer service department. Here's how to download the form:
- Visit the Carelon Rx website at .
- Click on the "Resources" tab and select "Prior Authorization Forms."
- Choose the correct form for your patient's medication and download the PDF file.
- Complete the form according to the instructions provided above.

FAQs
Here are some frequently asked questions about the Carelon Rx Prior Authorization Form:
Q: What is the purpose of the Carelon Rx Prior Authorization Form?
A: The Carelon Rx Prior Authorization Form is used to request prior authorization for prescription medications.
Q: How do I complete the Carelon Rx Prior Authorization Form?
A: Complete the form by entering the patient's information, prescriber information, medication information, medical condition, and treatment plan.
Q: Where can I download the Carelon Rx Prior Authorization Form?
A: The form can be downloaded from the Carelon Rx website or by contacting their customer service department.
Q: How long does it take to process the prior authorization request?
A: The processing time for prior authorization requests varies depending on the complexity of the request and the availability of necessary information.
Q: Can I submit the prior authorization request electronically?
A: Yes, Carelon Rx offers electronic submission options for prior authorization requests.
What happens if the prior authorization request is denied?
+If the prior authorization request is denied, the healthcare provider can appeal the decision by submitting additional information or clarifying the patient's medical condition.
Can I use the Carelon Rx Prior Authorization Form for all medications?
+No, the Carelon Rx Prior Authorization Form is specific to certain medications and treatments. Check with Carelon Rx to determine which medications require prior authorization.
The Carelon Rx Prior Authorization Form is an essential document that helps streamline the prior authorization process for prescription medications. By understanding the form and following the steps outlined above, healthcare providers can ensure that their patients receive the necessary medications while controlling healthcare costs. If you have any further questions or need assistance with the prior authorization process, contact Carelon Rx customer service department.
We hope this article has provided you with a comprehensive guide to the Carelon Rx Prior Authorization Form. If you have any further questions or would like to share your experiences with the prior authorization process, please leave a comment below.