Meridian prior authorization forms are a crucial part of the healthcare process, allowing providers to obtain approval for certain treatments or services before they are administered. With the ever-changing landscape of healthcare regulations and insurance policies, navigating the prior authorization process can be complex and time-consuming. In this article, we will explore five tips for Meridian prior authorization form success, highlighting the importance of clear communication, accurate documentation, and efficient submission processes.

Understanding the Importance of Prior Authorization
Prior authorization is a critical step in ensuring that patients receive the necessary care while also controlling healthcare costs. By obtaining approval before administering treatment, providers can avoid denied claims, reduce administrative burdens, and prevent delays in patient care. However, the prior authorization process can be lengthy and requires careful attention to detail, making it essential to understand the specific requirements and guidelines set forth by Meridian.
Tip 1: Clear Communication with Patients and Providers
Effective communication is vital when it comes to Meridian prior authorization forms. Providers must clearly explain the prior authorization process to patients, ensuring they understand the requirements and potential delays. This includes informing patients about the necessary documentation, expected timelines, and any additional steps that may be required. Similarly, providers must maintain open communication with Meridian, promptly responding to requests for additional information and addressing any concerns or issues that may arise during the process.
Benefits of Clear Communication
- Reduced patient anxiety and frustration
- Improved provider-patient relationships
- Enhanced collaboration between providers and Meridian
- Increased efficiency in the prior authorization process
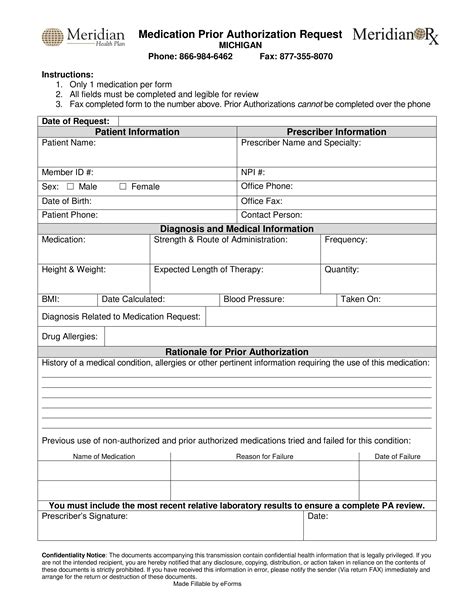
Tip 2: Accurate and Complete Documentation
Accurate and complete documentation is crucial when submitting Meridian prior authorization forms. Providers must ensure that all necessary information is included, such as patient demographics, medical history, and treatment details. Incomplete or inaccurate documentation can lead to delays, denials, or even claim rejections, emphasizing the importance of attention to detail.
Key Documentation Requirements
- Patient identification and demographics
- Medical history and diagnosis
- Treatment details, including medications and services
- Supporting documentation, such as test results and medical records

Tip 3: Efficient Submission Processes
Efficient submission processes are essential for streamlining the Meridian prior authorization process. Providers can utilize online portals or electronic submission systems to expedite the process, reducing paperwork and minimizing errors. Additionally, providers can take advantage of Meridian's customer support resources, such as phone support and online guides, to ensure timely and accurate submissions.
Benefits of Efficient Submission Processes
- Reduced administrative burdens
- Faster processing times
- Improved accuracy and reduced errors
- Enhanced provider satisfaction
Tip 4: Understanding Meridian's Guidelines and Requirements
Understanding Meridian's guidelines and requirements is critical for prior authorization form success. Providers must familiarize themselves with Meridian's policies, including specific requirements for documentation, submission processes, and deadlines. By staying up-to-date on Meridian's guidelines, providers can avoid common pitfalls and ensure a smoother prior authorization process.
Key Guidelines and Requirements
- Documentation requirements and submission processes
- Deadlines and timelines for prior authorization
- Specific policies and procedures for certain treatments or services

Tip 5: Leveraging Technology and Automation
Leveraging technology and automation can significantly improve the Meridian prior authorization process. Providers can utilize software solutions and electronic health records (EHRs) to streamline documentation, submission, and tracking. Additionally, providers can take advantage of automated workflows and reminders to ensure timely submissions and follow-ups.
Benefits of Technology and Automation
- Improved efficiency and productivity
- Reduced administrative burdens
- Enhanced accuracy and reduced errors
- Increased provider satisfaction

By implementing these five tips, providers can improve their chances of success with Meridian prior authorization forms. By maintaining clear communication, ensuring accurate documentation, and leveraging technology and automation, providers can streamline the prior authorization process, reduce administrative burdens, and improve patient outcomes.
We encourage you to share your experiences and insights on the Meridian prior authorization process in the comments below. Your feedback is invaluable in helping us better understand the challenges and opportunities in this complex and ever-changing landscape.
What is the purpose of prior authorization?
+Prior authorization is a process that allows healthcare providers to obtain approval for certain treatments or services before they are administered. This process helps control healthcare costs and ensures that patients receive necessary care.
What are the key requirements for Meridian prior authorization forms?
+The key requirements for Meridian prior authorization forms include accurate and complete documentation, clear communication with patients and providers, and efficient submission processes.
How can technology and automation improve the prior authorization process?
+Technology and automation can improve the prior authorization process by streamlining documentation, submission, and tracking. Additionally, automated workflows and reminders can ensure timely submissions and follow-ups.