Understanding the Meridian Outpatient Prior Authorization Form

Prior authorization is a critical step in the healthcare process, ensuring that patients receive necessary medical treatments while controlling healthcare costs. The Meridian Outpatient Prior Authorization Form is a crucial document used by healthcare providers to request approval for specific medical services or treatments. In this article, we will delve into the world of prior authorization, exploring the Meridian Outpatient Prior Authorization Form in detail.
What is Prior Authorization?
Prior authorization, also known as pre-authorization or pre-certification, is a process where healthcare providers obtain approval from a patient's insurance company before providing specific medical services or treatments. This process ensures that the requested services are medically necessary and meet the insurance company's coverage criteria. Prior authorization is commonly required for high-cost or specialized treatments, such as surgeries, imaging tests, or prescription medications.
Why is Prior Authorization Important?

Prior authorization plays a vital role in the healthcare system, serving several purposes:
- Cost control: Prior authorization helps insurance companies control healthcare costs by ensuring that only medically necessary services are approved.
- Quality of care: Prior authorization ensures that patients receive high-quality care by verifying that the requested services meet established medical standards.
- Patient safety: Prior authorization helps prevent unnecessary treatments or procedures that may pose risks to patients.
What is the Meridian Outpatient Prior Authorization Form?
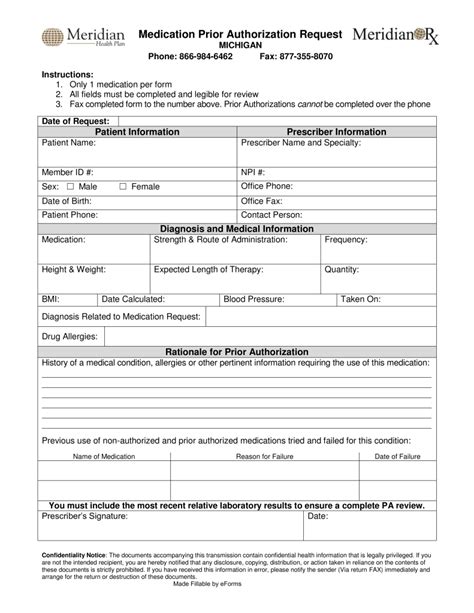
The Meridian Outpatient Prior Authorization Form is a document used by healthcare providers to request prior authorization for outpatient medical services. This form is specific to Meridian Health Plan, a Medicaid-managed care organization that operates in several states. The form requires healthcare providers to submit detailed information about the patient, the requested services, and the medical justification for the treatment.
How to Complete the Meridian Outpatient Prior Authorization Form

To complete the Meridian Outpatient Prior Authorization Form, healthcare providers must follow these steps:
- Patient information: Enter the patient's demographic information, including name, date of birth, and Medicaid ID number.
- Service information: Describe the requested medical services or treatments, including the procedure code, diagnosis code, and treatment date.
- Medical justification: Provide a detailed explanation of the medical necessity for the requested services, including relevant medical history and current symptoms.
- Supporting documentation: Attach relevant medical records, test results, or other supporting documentation to the form.
- Provider information: Enter the healthcare provider's information, including name, address, and contact details.
Tips for Successful Prior Authorization
To increase the chances of successful prior authorization, healthcare providers should:
- Submit complete and accurate information: Ensure that all required fields are completed, and the information is accurate and up-to-date.
- Provide thorough medical justification: Clearly explain the medical necessity for the requested services, using relevant medical terminology and documentation.
- Attach supporting documentation: Include all relevant medical records, test results, or other supporting documentation to support the prior authorization request.
Common Reasons for Prior Authorization Denials

Prior authorization requests can be denied due to various reasons, including:
- Incomplete or inaccurate information: Missing or incorrect information can lead to delays or denials.
- Lack of medical justification: Insufficient or unclear medical justification can result in denials.
- Non-compliance with insurance policies: Failure to comply with insurance policies or guidelines can lead to denials.
Appealing a Prior Authorization Denial
If a prior authorization request is denied, healthcare providers can appeal the decision by:
- Submitting additional information: Provide additional medical justification or supporting documentation to support the appeal.
- Requesting a peer-to-peer review: Request a review by a medical peer to re-evaluate the prior authorization request.
- Escalating the appeal: Escalate the appeal to a higher level of review, such as a committee or a senior reviewer.
What is the purpose of prior authorization?
+Prior authorization is a process that ensures that patients receive necessary medical treatments while controlling healthcare costs.
What is the Meridian Outpatient Prior Authorization Form?
+The Meridian Outpatient Prior Authorization Form is a document used by healthcare providers to request prior authorization for outpatient medical services.
What are common reasons for prior authorization denials?
+Prior authorization requests can be denied due to incomplete or inaccurate information, lack of medical justification, or non-compliance with insurance policies.
We hope this comprehensive guide to the Meridian Outpatient Prior Authorization Form has been informative and helpful. By understanding the prior authorization process and completing the form accurately, healthcare providers can ensure that their patients receive the necessary medical treatments while minimizing delays and denials. If you have any further questions or concerns, please don't hesitate to comment below or share this article with others.