Medicaid authorization forms are a crucial part of the Medicaid process in Florida, ensuring that patients receive the necessary medical care while also protecting the rights of healthcare providers. Understanding the Medicaid authorization form in Florida is essential for healthcare professionals, patients, and families to navigate the complex healthcare system. In this article, we will provide a step-by-step guide on the Medicaid authorization form in Florida, covering its importance, the process of obtaining authorization, and tips for successful submission.

What is a Medicaid Authorization Form in Florida?
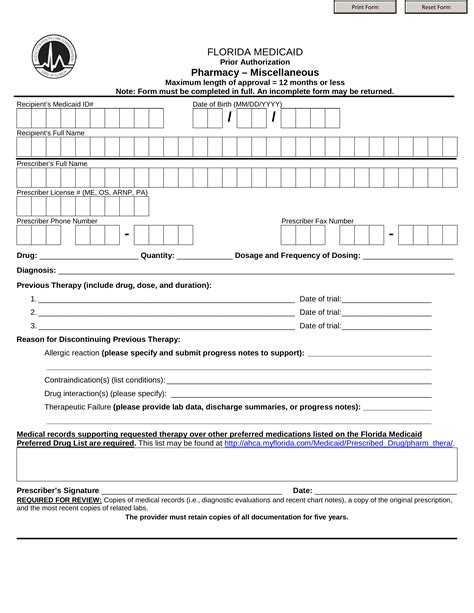
A Medicaid authorization form in Florida is a document that allows healthcare providers to obtain prior authorization for certain medical services, treatments, or equipment. The form is typically submitted to the Florida Medicaid program for review and approval before the provision of care. The primary purpose of the authorization form is to ensure that Medicaid beneficiaries receive medically necessary services while also controlling healthcare costs.
Benefits of Medicaid Authorization Form in Florida
The Medicaid authorization form in Florida offers several benefits, including:
- Ensures that patients receive medically necessary care
- Reduces the risk of denied claims and payment delays
- Streamlines the billing and reimbursement process
- Enhances patient care coordination and communication among healthcare providers
- Supports the overall goal of cost-effective healthcare delivery
Step-by-Step Guide to Medicaid Authorization Form in Florida
Obtaining Medicaid authorization in Florida involves several steps, which are outlined below:
Step 1: Verify Medicaid Eligibility
Before submitting the authorization form, healthcare providers must verify the patient's Medicaid eligibility. This can be done by contacting the Florida Medicaid program or using online tools, such as the Medicaid eligibility verification system.
Step 2: Determine the Need for Authorization
Not all medical services require prior authorization. Healthcare providers must review the Florida Medicaid program's guidelines and policies to determine if authorization is needed for a specific service or treatment.
Step 3: Gather Required Information
Healthcare providers must gather the necessary information and documentation to support the authorization request. This may include:
- Patient demographics and Medicaid identification number
- Service or treatment details, including dates and frequencies
- Medical records and supporting documentation
- Prescription information, if applicable
Step 4: Complete the Authorization Form
The Medicaid authorization form in Florida must be completed accurately and thoroughly. Healthcare providers should ensure that all required fields are filled in and that the form is signed and dated.

Step 5: Submit the Authorization Form
The completed authorization form must be submitted to the Florida Medicaid program for review and approval. Healthcare providers can submit the form via mail, fax, or online through the Medicaid portal.
Step 6: Receive Authorization Approval or Denial
The Florida Medicaid program will review the authorization request and notify the healthcare provider of the approval or denial decision. If approved, the provider will receive an authorization number, which must be included on the claim form.
Tips for Successful Medicaid Authorization Form Submission in Florida
To ensure successful submission of the Medicaid authorization form in Florida, healthcare providers should:
- Verify patient eligibility and review program guidelines before submitting the form
- Ensure accurate and complete information on the authorization form
- Include supporting documentation, such as medical records and prescriptions
- Submit the form well in advance of the scheduled service or treatment
- Follow up with the Medicaid program to confirm receipt and approval of the authorization request

Common Mistakes to Avoid When Submitting Medicaid Authorization Form in Florida
Common mistakes to avoid when submitting the Medicaid authorization form in Florida include:
- Incomplete or inaccurate information on the authorization form
- Failure to verify patient eligibility or review program guidelines
- Insufficient supporting documentation
- Late submission of the authorization form
- Failure to follow up with the Medicaid program to confirm receipt and approval
Conclusion
The Medicaid authorization form in Florida is a critical component of the Medicaid process, ensuring that patients receive medically necessary care while controlling healthcare costs. By following the step-by-step guide outlined above and avoiding common mistakes, healthcare providers can successfully submit the authorization form and provide high-quality care to Medicaid beneficiaries.
We encourage you to share your experiences and tips for navigating the Medicaid authorization process in Florida. Your feedback will help us improve our content and provide better support to healthcare professionals and patients.
What is the purpose of the Medicaid authorization form in Florida?
+The Medicaid authorization form in Florida allows healthcare providers to obtain prior authorization for certain medical services, treatments, or equipment, ensuring that patients receive medically necessary care while controlling healthcare costs.
How do I verify Medicaid eligibility in Florida?
+You can verify Medicaid eligibility in Florida by contacting the Florida Medicaid program or using online tools, such as the Medicaid eligibility verification system.
What information is required on the Medicaid authorization form in Florida?
+The Medicaid authorization form in Florida requires patient demographics, Medicaid identification number, service or treatment details, medical records, and supporting documentation.