Completing a Kentucky Medicaid prior authorization form can be a daunting task, especially for healthcare providers who are new to the process. However, with the right guidance, it can be a straightforward process that ensures patients receive the necessary treatment and care. In this article, we will break down the 7 essential steps to complete a Kentucky Medicaid prior authorization form successfully.
Understanding the Importance of Prior Authorization

Prior authorization is a critical process in the healthcare system that ensures patients receive necessary medical treatment while controlling healthcare costs. In Kentucky, Medicaid prior authorization is mandatory for certain medical procedures, medications, and services. The process involves healthcare providers submitting a prior authorization request to Kentucky Medicaid, which reviews the request to determine whether the treatment or service is medically necessary.
Benefits of Prior Authorization
Prior authorization offers several benefits to patients, healthcare providers, and the healthcare system as a whole. Some of the benefits include:
- Ensures patients receive medically necessary treatment
- Reduces healthcare costs by avoiding unnecessary treatments
- Improves patient outcomes by ensuring patients receive evidence-based treatments
- Enhances communication between healthcare providers and patients
Step 1: Determine if Prior Authorization is Required

The first step in completing a Kentucky Medicaid prior authorization form is to determine whether prior authorization is required for a specific treatment or service. Healthcare providers can check the Kentucky Medicaid website or consult with a prior authorization specialist to determine if prior authorization is necessary.
Prior Authorization Requirements
Prior authorization is typically required for:
- Certain medications, such as specialty medications or high-cost medications
- Medical procedures, such as surgeries or diagnostic tests
- Durable medical equipment (DME)
- Home health care services
Step 2: Gather Required Information and Documents

Once you have determined that prior authorization is required, the next step is to gather the necessary information and documents. This may include:
- Patient demographic information
- Medical history and diagnosis
- Treatment plan and medication list
- Supporting documentation, such as lab results or medical records
Required Documents
The following documents may be required to complete a prior authorization request:
- Completed prior authorization form
- Patient's medical records
- Lab results or test results
- Medication list
- Treatment plan
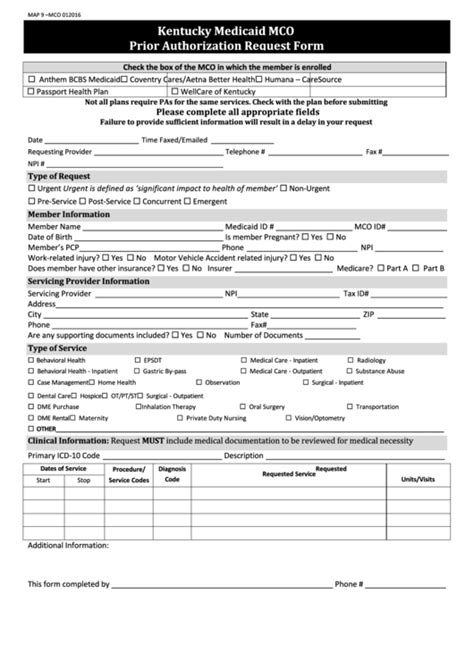
Step 3: Complete the Prior Authorization Form

The next step is to complete the prior authorization form. The form typically requires information about the patient, the treatment or service being requested, and the healthcare provider.
Prior Authorization Form Sections
The prior authorization form typically includes the following sections:
- Patient information
- Healthcare provider information
- Treatment or service information
- Supporting documentation
Step 4: Submit the Prior Authorization Request

Once the prior authorization form is complete, the next step is to submit the request to Kentucky Medicaid. This can be done electronically or by mail.
Prior Authorization Submission Methods
Prior authorization requests can be submitted:
- Electronically through the Kentucky Medicaid website
- By mail to the Kentucky Medicaid address
Step 5: Wait for Prior Authorization Approval

After submitting the prior authorization request, the next step is to wait for approval. Kentucky Medicaid will review the request to determine whether the treatment or service is medically necessary.
Prior Authorization Approval Timeline
The prior authorization approval timeline may vary depending on the complexity of the request. However, most requests are processed within 24-48 hours.
Step 6: Receive Prior Authorization Approval or Denial

Once the prior authorization request is reviewed, Kentucky Medicaid will send a decision letter to the healthcare provider. The letter will indicate whether the prior authorization request has been approved or denied.
Prior Authorization Decision Letter
The prior authorization decision letter will include:
- Approval or denial of the prior authorization request
- Reason for denial (if applicable)
- Instructions for next steps
Step 7: Follow Up on Prior Authorization Approval or Denial

The final step is to follow up on the prior authorization approval or denial. If the request is approved, the healthcare provider can proceed with the treatment or service. If the request is denied, the healthcare provider can appeal the decision or submit a new request.
Prior Authorization Follow-up
Follow-up may involve:
- Scheduling the approved treatment or service
- Appealing the denial decision
- Submitting a new prior authorization request
What is prior authorization?
+Prior authorization is a process that requires healthcare providers to obtain approval from Kentucky Medicaid before providing certain medical treatments or services.
Why is prior authorization required?
+Prior authorization is required to ensure that patients receive medically necessary treatment while controlling healthcare costs.
How long does prior authorization take?
+Prior authorization typically takes 24-48 hours to process.
By following these 7 essential steps, healthcare providers can successfully complete a Kentucky Medicaid prior authorization form and ensure that patients receive the necessary treatment and care. Remember to stay informed about prior authorization requirements and procedures to avoid delays or denials.