Kentucky Medicaid prior authorization can be a complex and time-consuming process for healthcare providers. The prior authorization process is designed to ensure that Medicaid beneficiaries receive medically necessary treatments and services while also controlling costs. However, the process can be lengthy and bureaucratic, causing frustration for both providers and patients. In this article, we will explore five ways to simplify Kentucky Medicaid prior authorization and make the process more efficient.
Understanding the Prior Authorization Process

Before we dive into the ways to simplify the prior authorization process, it's essential to understand how it works. The prior authorization process typically involves the following steps:
- The healthcare provider submits a request for prior authorization to the Medicaid managed care organization (MCO) or the Kentucky Medicaid program.
- The MCO or Medicaid program reviews the request to determine whether the treatment or service is medically necessary.
- If the request is approved, the provider receives an authorization number, which is required for reimbursement.
- If the request is denied, the provider can appeal the decision.
1. Implement Electronic Prior Authorization

One way to simplify the prior authorization process is to implement electronic prior authorization (ePA). ePA allows providers to submit prior authorization requests electronically, reducing paperwork and administrative burdens. ePA systems can also automate the review process, reducing the time it takes to receive an authorization decision.
- Benefits of ePA:
- Reduced administrative burdens
- Faster authorization decisions
- Improved accuracy and reduced errors
- Examples of ePA systems:
- CoverMyMeds
- Surescripts
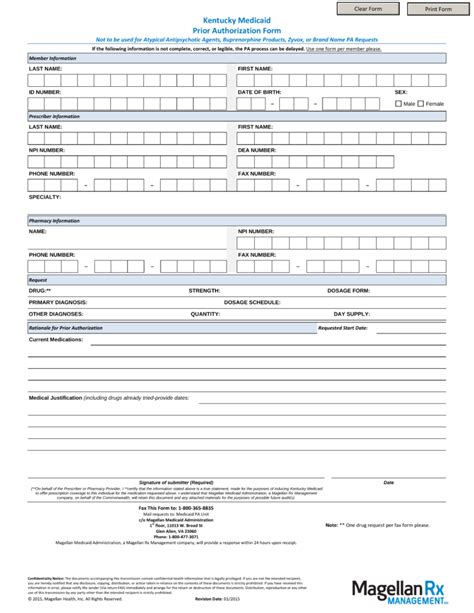
2. Streamline the Prior Authorization Form

Another way to simplify the prior authorization process is to streamline the prior authorization form. The form should be easy to understand and complete, with clear instructions and minimal required fields.
- Benefits of a streamlined form:
- Reduced provider burden
- Improved accuracy and reduced errors
- Faster authorization decisions
- Tips for streamlining the form:
- Use clear and concise language
- Reduce the number of required fields
- Use checkboxes and dropdown menus instead of free-text fields
3. Implement a Prior Authorization Dashboard

A prior authorization dashboard can help simplify the prior authorization process by providing a centralized location for tracking and managing prior authorization requests.
- Benefits of a dashboard:
- Improved visibility and tracking
- Reduced administrative burdens
- Faster authorization decisions
- Features of a dashboard:
- Real-time tracking and updates
- Customizable reporting and analytics
- Secure and HIPAA-compliant
4. Develop a Prior Authorization Guide

A prior authorization guide can help simplify the prior authorization process by providing a comprehensive resource for providers.
- Benefits of a guide:
- Improved understanding and compliance
- Reduced provider burden
- Faster authorization decisions
- Features of a guide:
- Clear and concise language
- Step-by-step instructions
- Frequently asked questions (FAQs)
5. Provide Prior Authorization Training

Providing prior authorization training can help simplify the prior authorization process by educating providers on the requirements and procedures.
- Benefits of training:
- Improved understanding and compliance
- Reduced provider burden
- Faster authorization decisions
- Types of training:
- Webinars
- Online tutorials
- In-person workshops
By implementing these five strategies, healthcare providers and Medicaid managed care organizations can simplify the prior authorization process and reduce administrative burdens.
What's Next?
We hope this article has provided valuable insights and strategies for simplifying the Kentucky Medicaid prior authorization process. If you have any questions or comments, please don't hesitate to reach out. Share this article with your colleagues and peers to help spread the word about the importance of simplifying prior authorization.
What is prior authorization?
+Prior authorization is a process used by Medicaid managed care organizations and the Kentucky Medicaid program to determine whether a treatment or service is medically necessary before it is provided.
Why is prior authorization necessary?
+Prior authorization is necessary to ensure that Medicaid beneficiaries receive medically necessary treatments and services while also controlling costs.
How can I simplify the prior authorization process?
+You can simplify the prior authorization process by implementing electronic prior authorization, streamlining the prior authorization form, using a prior authorization dashboard, developing a prior authorization guide, and providing prior authorization training.