Kaiser Permanente is one of the largest and most well-known health plans in the United States, serving millions of members across the country. As a healthcare provider, Kaiser Permanente strives to deliver high-quality, patient-centered care while also managing costs and ensuring that medical services are delivered in a responsible and sustainable manner. One way Kaiser Permanente achieves this is through the use of prior authorization forms, which are an essential part of the healthcare process in California. In this comprehensive guide, we will walk you through the Kaiser Permanente prior authorization form process in California, highlighting key aspects, benefits, and best practices.
Understanding Prior Authorization
Prior authorization is a process by which healthcare providers and insurance companies verify the medical necessity of certain treatments, procedures, or medications before they are administered. This helps ensure that patients receive safe, effective, and necessary care while also controlling healthcare costs. Prior authorization is an essential tool in managed care, as it allows healthcare organizations to assess the medical necessity of services and prevent unnecessary or wasteful spending.
Why is Prior Authorization Important in California?
Prior authorization is crucial in California, where healthcare costs are among the highest in the nation. By verifying the medical necessity of treatments and services, prior authorization helps prevent unnecessary or ineffective care, which can drive up costs and compromise patient outcomes. In California, prior authorization is required for certain medical services, including prescription medications, surgical procedures, and hospital admissions.
Kaiser Permanente Prior Authorization Process
Kaiser Permanente's prior authorization process is designed to ensure that members receive medically necessary care while minimizing unnecessary or wasteful spending. Here's an overview of the process:
- Request for Prior Authorization: Healthcare providers submit a request for prior authorization to Kaiser Permanente, providing detailed information about the proposed treatment or service, including medical necessity, patient diagnosis, and treatment plan.
- Review and Evaluation: Kaiser Permanente's clinical staff reviews and evaluates the request, assessing medical necessity and adherence to evidence-based guidelines and clinical protocols.
- Approval or Denial: Kaiser Permanente renders a decision, either approving or denying the request. If approved, the authorization is typically valid for a specific period.
- Appeals Process: If a request is denied, providers or members can appeal the decision, providing additional information or supporting documentation.

Benefits of Prior Authorization
Prior authorization offers several benefits for Kaiser Permanente members, healthcare providers, and the healthcare system as a whole. Some of the key advantages include:
- Improved Patient Outcomes: Prior authorization ensures that patients receive medically necessary care, which can lead to better health outcomes and reduced complications.
- Reduced Healthcare Costs: By preventing unnecessary or ineffective care, prior authorization helps control healthcare costs and reduces waste.
- Enhanced Quality of Care: Prior authorization promotes adherence to evidence-based guidelines and clinical protocols, leading to higher-quality care.
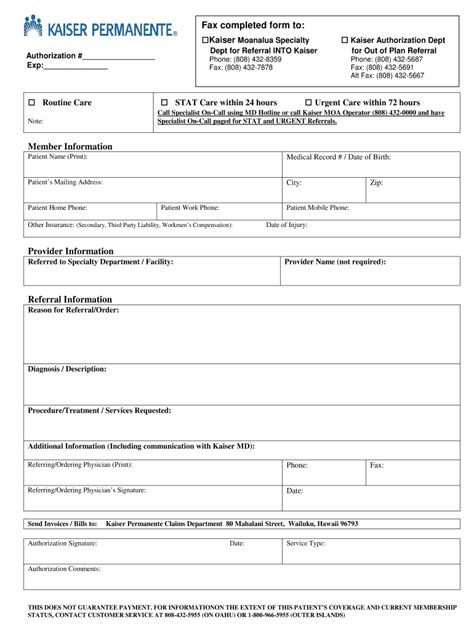
Common Kaiser Permanente Prior Authorization Forms
Kaiser Permanente uses various prior authorization forms, depending on the specific service or treatment. Some common forms include:
- Medication Prior Authorization Form: Used for prescription medications, this form requires healthcare providers to provide detailed information about the medication, patient diagnosis, and treatment plan.
- Surgical Prior Authorization Form: Used for surgical procedures, this form requires healthcare providers to provide information about the procedure, patient diagnosis, and treatment plan.
- Hospital Admission Prior Authorization Form: Used for hospital admissions, this form requires healthcare providers to provide information about the patient's condition, treatment plan, and expected length of stay.
Tips for Completing Kaiser Permanente Prior Authorization Forms
Completing prior authorization forms accurately and thoroughly is essential for ensuring that requests are processed efficiently and effectively. Here are some tips for completing Kaiser Permanente prior authorization forms:
- Read and Follow Instructions Carefully: Ensure that you understand the requirements and instructions for each form.
- Provide Complete and Accurate Information: Include all necessary information, such as patient diagnosis, treatment plan, and supporting documentation.
- Use Clear and Concise Language: Avoid using jargon or technical terms that may be unfamiliar to Kaiser Permanente staff.
- Submit Requests Electronically: Whenever possible, submit requests electronically to reduce processing time and improve efficiency.
Common Challenges and Solutions
Despite the importance of prior authorization, healthcare providers and Kaiser Permanente members may encounter challenges and delays in the process. Here are some common issues and potential solutions:
- Delays in Processing: Ensure that requests are submitted electronically and include all necessary information to reduce processing time.
- Denials and Appeals: Understand the appeals process and provide additional information or supporting documentation to support the request.
- Lack of Transparency: Contact Kaiser Permanente's customer service or clinical staff to clarify requirements and obtain updates on the status of requests.

Best Practices for Kaiser Permanente Prior Authorization
To ensure that the prior authorization process runs smoothly and efficiently, healthcare providers and Kaiser Permanente members should follow these best practices:
- Stay Informed: Familiarize yourself with Kaiser Permanente's prior authorization policies and procedures.
- Plan Ahead: Submit requests well in advance of the proposed treatment or service.
- Communicate Effectively: Ensure that all parties, including healthcare providers, patients, and Kaiser Permanente staff, are informed and up-to-date on the status of requests.
Conclusion and Next Steps
Prior authorization is a critical component of the healthcare process in California, and Kaiser Permanente's prior authorization form process is designed to ensure that members receive medically necessary care while controlling costs. By understanding the prior authorization process, benefits, and best practices, healthcare providers and Kaiser Permanente members can work together to improve patient outcomes and reduce healthcare costs. If you have questions or concerns about the prior authorization process, don't hesitate to contact Kaiser Permanente's customer service or clinical staff for assistance.
What's Next?
- Stay Informed: Check Kaiser Permanente's website for updates on prior authorization policies and procedures.
- Contact Kaiser Permanente: Reach out to Kaiser Permanente's customer service or clinical staff for assistance with prior authorization requests.
- Provide Feedback: Share your experiences and suggestions for improving the prior authorization process.
What is prior authorization, and why is it necessary?
+Prior authorization is a process by which healthcare providers and insurance companies verify the medical necessity of certain treatments, procedures, or medications before they are administered. It's necessary to ensure that patients receive safe, effective, and necessary care while controlling healthcare costs.
How do I submit a prior authorization request to Kaiser Permanente?
+You can submit a prior authorization request to Kaiser Permanente electronically or by phone. Ensure that you include all necessary information, such as patient diagnosis, treatment plan, and supporting documentation.
What if my prior authorization request is denied?
+If your prior authorization request is denied, you can appeal the decision by providing additional information or supporting documentation. Understand the appeals process and contact Kaiser Permanente's customer service or clinical staff for assistance.