IngenioRx prior authorization fax form can be a daunting task for many healthcare professionals. The process of obtaining prior authorization for medications can be complex and time-consuming, but it's a necessary step to ensure that patients receive the right treatment. In this article, we'll break down the IngenioRx prior authorization fax form process and provide tips to make it easier.
Understanding the Importance of Prior Authorization
Prior authorization is a process that requires healthcare providers to obtain approval from a patient's insurance company before prescribing certain medications. This process helps ensure that patients receive medically necessary treatment while also controlling healthcare costs. IngenioRx, a leading pharmacy benefit management company, requires prior authorization for certain medications to ensure that patients receive the most effective and cost-efficient treatment.

The IngenioRx Prior Authorization Fax Form Process
The IngenioRx prior authorization fax form process involves several steps that healthcare providers must follow to obtain approval for certain medications. Here's an overview of the process:
- Determine if prior authorization is required: Healthcare providers must check the IngenioRx formulary to determine if prior authorization is required for a specific medication.
- Gather required information: Healthcare providers must gather all required information, including patient demographics, medical history, and medication details.
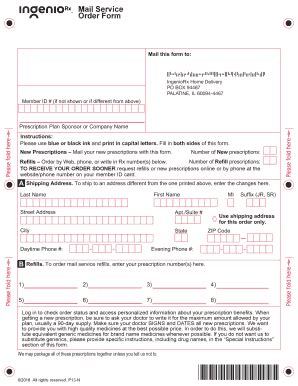
- Complete the prior authorization fax form: Healthcare providers must complete the IngenioRx prior authorization fax form, which includes providing detailed information about the patient and the medication being prescribed.
- Fax the form to IngenioRx: Healthcare providers must fax the completed form to IngenioRx, along with any supporting documentation.
Tips for Completing the IngenioRx Prior Authorization Fax Form
Completing the IngenioRx prior authorization fax form can be a time-consuming process, but there are several tips that healthcare providers can follow to make it easier:
- Use the correct form: Make sure to use the correct IngenioRx prior authorization fax form, which can be found on the company's website.
- Provide complete and accurate information: Make sure to provide complete and accurate information about the patient and the medication being prescribed.
- Include supporting documentation: Include any supporting documentation, such as medical records or test results, to support the request for prior authorization.
- Fax the form to the correct number: Make sure to fax the form to the correct number, which can be found on the IngenioRx website.

Common Challenges with the IngenioRx Prior Authorization Fax Form Process
Despite the best efforts of healthcare providers, there are several common challenges that can arise during the IngenioRx prior authorization fax form process. Here are some of the most common challenges:
- Incomplete or inaccurate information: Providing incomplete or inaccurate information can delay or even deny prior authorization.
- Supporting documentation: Failing to include supporting documentation can delay or even deny prior authorization.
- Technical issues: Technical issues, such as fax machine problems, can delay or even deny prior authorization.
Overcoming Common Challenges
There are several ways that healthcare providers can overcome common challenges with the IngenioRx prior authorization fax form process:
- Double-check information: Double-check information to ensure that it is complete and accurate.
- Include all supporting documentation: Include all supporting documentation to support the request for prior authorization.
- Use a reliable fax machine: Use a reliable fax machine to ensure that the form is transmitted correctly.

The Benefits of Using the IngenioRx Prior Authorization Fax Form
Despite the challenges, there are several benefits to using the IngenioRx prior authorization fax form process:
- Improved patient outcomes: Prior authorization can help ensure that patients receive the most effective treatment, leading to improved patient outcomes.
- Reduced healthcare costs: Prior authorization can help control healthcare costs by ensuring that patients receive medically necessary treatment.
- Streamlined process: The IngenioRx prior authorization fax form process can help streamline the process of obtaining prior authorization, making it easier for healthcare providers to focus on patient care.
Conclusion
The IngenioRx prior authorization fax form process can be complex and time-consuming, but it's a necessary step to ensure that patients receive the right treatment. By following the tips outlined in this article, healthcare providers can make the process easier and overcome common challenges. Remember, the benefits of using the IngenioRx prior authorization fax form process, including improved patient outcomes and reduced healthcare costs, make it an essential part of patient care.

What is prior authorization?
+Prior authorization is a process that requires healthcare providers to obtain approval from a patient's insurance company before prescribing certain medications.
Why is prior authorization required?
+Prior authorization is required to ensure that patients receive medically necessary treatment while also controlling healthcare costs.
How do I complete the IngenioRx prior authorization fax form?
+Complete the IngenioRx prior authorization fax form by providing detailed information about the patient and the medication being prescribed, and include any supporting documentation.