The IEHP Authorization Form is a crucial document for healthcare providers seeking reimbursement for medical services rendered to patients enrolled in the Inland Empire Health Plan (IEHP). Securing approval for this form can be a daunting task, but with a clear understanding of the process and a step-by-step approach, providers can increase their chances of successful authorization. In this article, we will outline the 5 easy steps to IEHP authorization form approval, making it easier for healthcare providers to navigate the process.
Understanding the Importance of IEHP Authorization
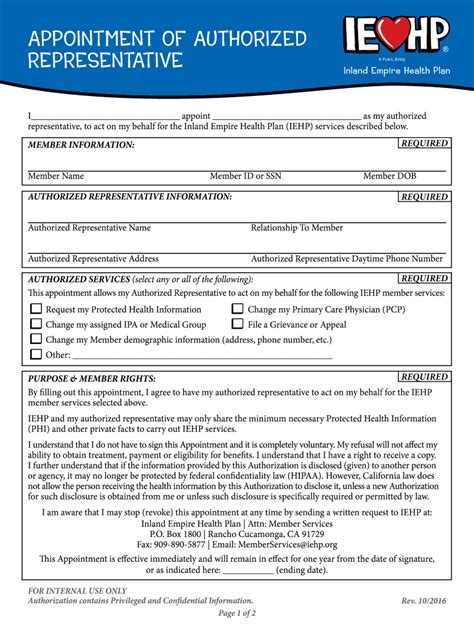
Before diving into the steps, it's essential to understand the significance of the IEHP Authorization Form. This form serves as a request for approval from IEHP to provide specific medical services to patients. The form requires detailed information about the patient, the services being requested, and the provider's credentials. Without proper authorization, providers risk delayed or denied reimbursement, which can impact their bottom line and patient care.

Step 1: Verify Patient Eligibility
The first step in the authorization process is to verify the patient's eligibility for IEHP coverage. Providers can check the patient's eligibility through the IEHP website or by contacting the IEHP Customer Service department directly. This step is crucial, as it ensures that the patient is actively enrolled in the plan and eligible for the requested services.
- Verify patient eligibility through the IEHP website or by contacting Customer Service
- Confirm patient's enrollment status and coverage dates
- Ensure patient meets the plan's requirements for the requested services
Step 2: Gather Required Documentation
Once patient eligibility is confirmed, providers must gather all required documentation to support the authorization request. This includes:
-
Patient demographics and contact information
-
Medical records and treatment plans
-
Provider credentials and licensure
-
Detailed description of services being requested
-
Supporting documentation, such as lab results or medical images
-
Collect and review all required documentation to ensure accuracy and completeness
-
Ensure documentation meets IEHP's requirements and guidelines
-
Organize documentation in a clear and concise manner for easy review
Step 3: Complete the Authorization Form
With all documentation in hand, providers can complete the IEHP Authorization Form. The form requires detailed information about the patient, services being requested, and provider credentials. Providers must ensure that the form is completed accurately and thoroughly, as incomplete or inaccurate information can lead to delayed or denied authorization.
- Complete the authorization form in its entirety, ensuring accuracy and completeness
- Attach all required documentation to support the authorization request
- Ensure provider credentials and licensure are up-to-date and accurate
Step 4: Submit the Authorization Request
Once the authorization form is complete, providers can submit the request to IEHP. Providers can submit the request via fax, email, or through the IEHP website. It's essential to follow IEHP's submission guidelines to ensure timely processing.
- Submit the authorization request via fax, email, or through the IEHP website
- Ensure submission meets IEHP's guidelines and deadlines
- Verify receipt of the authorization request by IEHP
Step 5: Follow Up and Respond to Requests
After submitting the authorization request, providers should follow up with IEHP to ensure timely processing. Providers may be required to respond to additional requests for information or clarification. It's essential to respond promptly to these requests to avoid delays in the authorization process.
- Follow up with IEHP to ensure timely processing of the authorization request
- Respond promptly to requests for additional information or clarification
- Verify authorization approval and ensure reimbursement is processed correctly

Conclusion
Securing approval for the IEHP Authorization Form can be a complex process, but by following these 5 easy steps, healthcare providers can increase their chances of successful authorization. Remember to verify patient eligibility, gather required documentation, complete the authorization form, submit the request, and follow up with IEHP to ensure timely processing. By following these steps, providers can ensure that their patients receive the necessary medical services while minimizing delays and denied reimbursement.
Now, we invite you to share your thoughts and experiences with the IEHP authorization process. Have you encountered any challenges or successes? Share your comments below, and let's start a conversation!
What is the IEHP Authorization Form?
+The IEHP Authorization Form is a document required by Inland Empire Health Plan (IEHP) for healthcare providers to request approval for specific medical services rendered to patients enrolled in the plan.
How do I verify patient eligibility for IEHP coverage?
+Providers can verify patient eligibility through the IEHP website or by contacting the IEHP Customer Service department directly.
What documentation is required to support the authorization request?
+Required documentation includes patient demographics and contact information, medical records and treatment plans, provider credentials and licensure, and detailed description of services being requested.