Understanding the Importance of Highmark Provider Appeal Form

As a healthcare provider, you understand the significance of a well-structured appeal process in ensuring that your claims are accurately reimbursed. One crucial document in this process is the Highmark Provider Appeal Form. This form serves as a crucial tool for providers to contest denied claims, incorrect payments, or other adverse decisions made by Highmark. In this article, we will guide you through the four easy steps to achieve success with the Highmark Provider Appeal Form.
Why Is the Highmark Provider Appeal Form Important?

The Highmark Provider Appeal Form is essential for several reasons. Firstly, it allows providers to formally dispute denied claims, which can lead to significant revenue losses if not addressed promptly. Secondly, the appeal process ensures that providers receive fair reimbursement for their services, which is crucial for maintaining a sustainable healthcare practice. Lastly, the form helps to identify and rectify any errors or discrepancies in the claims process, ultimately improving the efficiency of the healthcare system.
Benefits of Using the Highmark Provider Appeal Form
The Highmark Provider Appeal Form offers several benefits to healthcare providers, including:
- A standardized and structured process for appealing denied claims
- A clear and transparent review process for appeals
- Opportunities for providers to provide additional information and context to support their appeal
- A formal channel for addressing grievances and resolving disputes
4 Easy Steps to Highmark Provider Appeal Form Success

To achieve success with the Highmark Provider Appeal Form, follow these four easy steps:
Step 1: Review and Understand the Denial Letter
Understanding the Denial Letter
Upon receiving a denial letter from Highmark, it is essential to carefully review the contents to understand the reasons for the denial. The letter should provide clear explanations for the denial, including any relevant policy or procedural information. Take note of the specific codes, policies, or rules cited in the denial letter, as these will be crucial in crafting your appeal.
Step 2: Gather Supporting Documentation
Collecting Relevant Information and Documentation
To build a strong appeal, gather all relevant information and documentation that supports your claim. This may include:
- Patient records and medical history
- Treatment plans and documentation
- Billing and coding information
- Correspondence with Highmark regarding the claim
Ensure that all documentation is accurate, complete, and up-to-date to avoid any delays or complications in the appeal process.
Step 3: Complete the Highmark Provider Appeal Form
Completing the Appeal Form
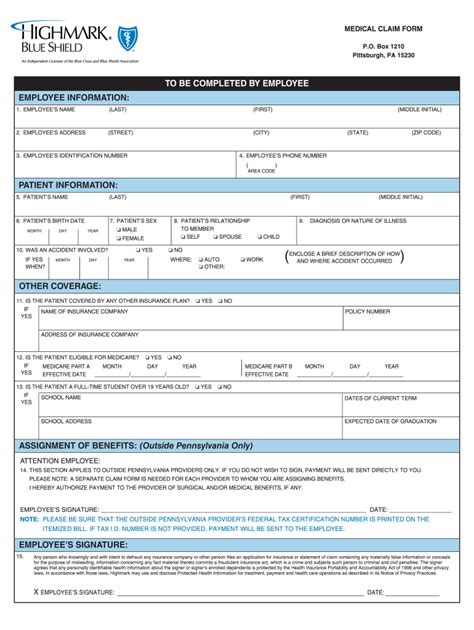
Once you have gathered all necessary documentation, complete the Highmark Provider Appeal Form. The form should include:
- Claim information, including the date of service and claim number
- A clear and concise explanation of the appeal, including any relevant policy or procedural information
- Supporting documentation, as outlined in Step 2
Ensure that the form is completed accurately and thoroughly, as any errors or omissions may result in delays or denials.
Step 4: Submit the Appeal Form and Supporting Documentation
Submitting the Appeal Form and Supporting Documentation
Once the appeal form is complete, submit it to Highmark along with all supporting documentation. Ensure that the appeal is submitted within the designated timeframe, as outlined in the denial letter or Highmark's policy.
Best Practices for Highmark Provider Appeal Form Success

To achieve success with the Highmark Provider Appeal Form, follow these best practices:
- Ensure that the appeal form is complete and accurate
- Provide clear and concise explanations for the appeal
- Include all relevant supporting documentation
- Submit the appeal within the designated timeframe
- Follow up with Highmark to ensure that the appeal is being processed
Conclusion
The Highmark Provider Appeal Form is a crucial tool for healthcare providers to contest denied claims and ensure fair reimbursement for their services. By following the four easy steps outlined in this article, providers can achieve success with the appeal form and minimize revenue losses. Remember to review and understand the denial letter, gather supporting documentation, complete the appeal form accurately, and submit the appeal within the designated timeframe. By doing so, you can ensure a smooth and successful appeal process.
What is the purpose of the Highmark Provider Appeal Form?
+The Highmark Provider Appeal Form is used to contest denied claims, incorrect payments, or other adverse decisions made by Highmark.
What information should I include in the Highmark Provider Appeal Form?
+The appeal form should include claim information, a clear and concise explanation of the appeal, and supporting documentation.
How long do I have to submit the Highmark Provider Appeal Form?
+The timeframe for submitting the appeal form varies, but it is typically outlined in the denial letter or Highmark's policy.