The process of obtaining prior authorization for medical procedures and medications can be daunting, especially for patients who are already dealing with health issues. Highmark, a leading health insurance provider, has its own prior authorization form that must be completed and submitted before certain treatments can be approved. In this article, we will break down the Highmark prior authorization form and provide a step-by-step guide on how to complete it.

What is Prior Authorization?
Prior authorization, also known as pre-certification or pre-authorization, is the process of obtaining approval from a health insurance provider before a medical procedure or medication can be administered. This process is designed to ensure that the treatment is medically necessary and that the patient's insurance plan covers the costs. Prior authorization can help prevent unnecessary medical expenses and reduce the risk of surprise medical bills.
Why is Prior Authorization Required?
Prior authorization is required for a variety of reasons, including:
- To ensure that the treatment is medically necessary and aligns with the patient's insurance plan
- To verify that the treatment is covered under the patient's insurance plan
- To prevent unnecessary medical expenses
- To reduce the risk of surprise medical bills
- To ensure that the patient receives the most effective and cost-efficient treatment
Highmark Prior Authorization Form: What You Need to Know
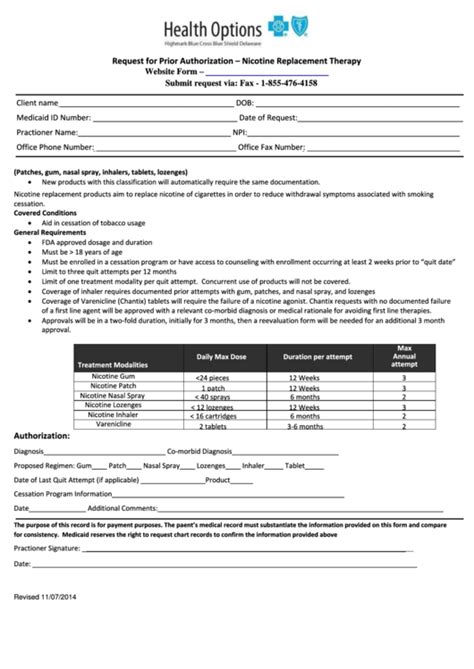
The Highmark prior authorization form is a document that must be completed and submitted before certain treatments can be approved. The form requires information about the patient, the treatment, and the provider. Here's what you need to know:
- The form must be completed by the patient's healthcare provider
- The form requires information about the patient's medical history, including any relevant diagnoses and treatments
- The form requires information about the treatment, including the type of treatment, the dosage, and the frequency
- The form requires information about the provider, including their name, address, and contact information

Step-by-Step Guide to Completing the Highmark Prior Authorization Form
Completing the Highmark prior authorization form can be a daunting task, but with our step-by-step guide, you'll be able to navigate the process with ease. Here's how to complete the form:
Step 1: Gather Required Information
Before you start completing the form, make sure you have all the required information. This includes:
- Patient information, including name, date of birth, and insurance ID number
- Medical history, including any relevant diagnoses and treatments
- Treatment information, including the type of treatment, the dosage, and the frequency
- Provider information, including name, address, and contact information
Step 2: Complete Section 1: Patient Information
Section 1 of the form requires patient information, including name, date of birth, and insurance ID number. Make sure to complete this section accurately and thoroughly.
Step 3: Complete Section 2: Medical History
Section 2 of the form requires information about the patient's medical history, including any relevant diagnoses and treatments. Make sure to include all relevant information, including dates and details of previous treatments.
Step 4: Complete Section 3: Treatment Information
Section 3 of the form requires information about the treatment, including the type of treatment, the dosage, and the frequency. Make sure to include all relevant information, including any relevant medical codes.
Step 5: Complete Section 4: Provider Information
Section 4 of the form requires information about the provider, including name, address, and contact information. Make sure to complete this section accurately and thoroughly.
Step 6: Review and Submit the Form
Once you've completed all sections of the form, review it carefully to ensure that all information is accurate and complete. Sign and date the form, and submit it to Highmark for review.

What to Expect After Submitting the Form
After submitting the Highmark prior authorization form, you can expect to receive a decision from Highmark within a few days. If the treatment is approved, you'll receive a letter or email notification with details about the approved treatment. If the treatment is denied, you'll receive a letter or email notification with details about the denial and any next steps.
Appealing a Denied Prior Authorization
If your prior authorization is denied, you have the right to appeal the decision. To appeal, you'll need to submit a written request to Highmark, including any additional information or documentation that supports your appeal. Highmark will review your appeal and make a decision within a few days.

Conclusion
The Highmark prior authorization form can be a daunting task, but with our step-by-step guide, you'll be able to navigate the process with ease. Remember to gather all required information, complete each section accurately and thoroughly, and review and submit the form carefully. If your prior authorization is denied, don't hesitate to appeal the decision. With the right information and support, you can ensure that you receive the medical treatment you need.
What is prior authorization?
+Prior authorization, also known as pre-certification or pre-authorization, is the process of obtaining approval from a health insurance provider before a medical procedure or medication can be administered.
Why is prior authorization required?
+Prior authorization is required to ensure that the treatment is medically necessary and aligns with the patient's insurance plan, to verify that the treatment is covered under the patient's insurance plan, and to prevent unnecessary medical expenses.
What happens after submitting the Highmark prior authorization form?
+After submitting the Highmark prior authorization form, you can expect to receive a decision from Highmark within a few days. If the treatment is approved, you'll receive a letter or email notification with details about the approved treatment. If the treatment is denied, you'll receive a letter or email notification with details about the denial and any next steps.