The complexities of the healthcare system can be overwhelming, especially when it comes to medication prior authorization. The Highmark Medication Prior Authorization Form is a crucial step in ensuring that patients receive the necessary medications while also controlling healthcare costs. In this article, we will delve into the world of prior authorization, explain the Highmark Medication Prior Authorization Form, and provide a step-by-step guide on how to complete it with ease.
The Importance of Prior Authorization
Prior authorization is a process used by health insurance companies to determine whether a specific medication or treatment is medically necessary and covered under a patient's insurance plan. This process helps to prevent unnecessary healthcare spending, ensures that patients receive the most effective treatments, and reduces the risk of adverse reactions. In the United States, prior authorization is a mandatory step for many prescription medications, including those used to treat chronic conditions such as diabetes, hypertension, and asthma.
What is the Highmark Medication Prior Authorization Form?

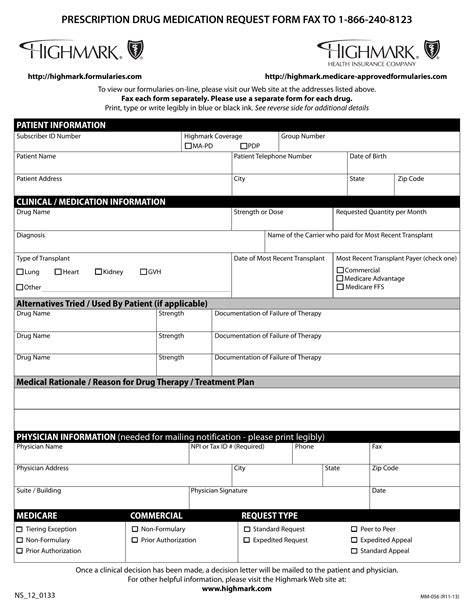
The Highmark Medication Prior Authorization Form is a document used by healthcare providers to request prior authorization for medications from Highmark, a leading health insurance company. The form requires providers to submit detailed information about the patient's medical condition, treatment history, and the requested medication. This information helps Highmark's clinical reviewers to determine whether the medication is medically necessary and covered under the patient's insurance plan.
Benefits of the Highmark Medication Prior Authorization Form

The Highmark Medication Prior Authorization Form offers several benefits to both healthcare providers and patients. Some of the key benefits include:
- Improved patient outcomes: By ensuring that patients receive the most effective medications, prior authorization helps to improve treatment outcomes and reduce the risk of adverse reactions.
- Reduced healthcare costs: Prior authorization helps to prevent unnecessary healthcare spending by ensuring that medications are only prescribed when medically necessary.
- Streamlined communication: The Highmark Medication Prior Authorization Form provides a standardized template for communication between healthcare providers and Highmark, reducing the risk of errors and miscommunication.
Step-by-Step Guide to Completing the Highmark Medication Prior Authorization Form

Completing the Highmark Medication Prior Authorization Form requires careful attention to detail and accurate information. Here is a step-by-step guide to help you complete the form with ease:
- Section 1: Patient Information: Enter the patient's demographic information, including name, date of birth, and insurance ID number.
- Section 2: Medication Information: Enter the name of the requested medication, dosage, and frequency of administration.
- Section 3: Medical Condition: Enter the patient's medical condition or diagnosis that requires the requested medication.
- Section 4: Treatment History: Enter the patient's treatment history, including any previous medications or treatments.
- Section 5: Clinical Rationale: Enter the clinical rationale for the requested medication, including any relevant medical literature or guidelines.
- Section 6: Supporting Documentation: Attach any supporting documentation, including lab results, medical records, or letters of medical necessity.
Tips and Tricks for a Smooth Prior Authorization Process

To ensure a smooth prior authorization process, follow these tips and tricks:
- Submit the completed form with all required documentation to avoid delays.
- Use the online portal or fax the form to ensure timely receipt.
- Include a clear and concise clinical rationale to support the requested medication.
- Attach all relevant supporting documentation to avoid requests for additional information.
- Follow up with Highmark to ensure that the prior authorization request is being processed.
Common Mistakes to Avoid When Completing the Highmark Medication Prior Authorization Form

When completing the Highmark Medication Prior Authorization Form, avoid the following common mistakes:
- Incomplete or inaccurate patient information.
- Missing or incomplete medication information.
- Failure to provide a clear and concise clinical rationale.
- Insufficient or irrelevant supporting documentation.
- Failure to follow up with Highmark to ensure timely processing.
By following these tips and avoiding common mistakes, you can ensure a smooth prior authorization process and help your patients receive the necessary medications in a timely manner.
Conclusion: Simplifying the Prior Authorization Process

The Highmark Medication Prior Authorization Form may seem complex, but by breaking it down into smaller sections and following a step-by-step guide, you can simplify the prior authorization process. Remember to avoid common mistakes, follow tips and tricks, and submit the completed form with all required documentation to ensure a smooth and timely process.
By taking the time to understand the Highmark Medication Prior Authorization Form and following the guidelines outlined in this article, you can help your patients receive the necessary medications while also controlling healthcare costs. Don't let the complexities of prior authorization overwhelm you – take the first step towards simplifying the process today!
What is the purpose of the Highmark Medication Prior Authorization Form?
+The Highmark Medication Prior Authorization Form is used to request prior authorization for medications from Highmark, a leading health insurance company. The form requires healthcare providers to submit detailed information about the patient's medical condition, treatment history, and the requested medication.
What are the benefits of the Highmark Medication Prior Authorization Form?
+The Highmark Medication Prior Authorization Form offers several benefits, including improved patient outcomes, reduced healthcare costs, and streamlined communication between healthcare providers and Highmark.
What are the common mistakes to avoid when completing the Highmark Medication Prior Authorization Form?
+