Navigating the Prior Authorization Process with Highmark BCBS
Prior authorization, also known as pre-certification or pre-authorization, is a critical step in ensuring that patients receive necessary medical treatments while controlling healthcare costs. Highmark Blue Cross Blue Shield (BCBS), one of the largest health insurance providers in the United States, requires prior authorization for certain medical procedures and medications. In this article, we will delve into the Highmark BCBS prior authorization form, its requirements, and provide a simplified guide to help healthcare providers and patients navigate the process.
Understanding the Importance of Prior Authorization
Prior authorization is a crucial step in ensuring that patients receive medically necessary treatments while controlling healthcare costs. By requiring prior authorization, Highmark BCBS can assess the medical necessity of a treatment or procedure, reducing the likelihood of unnecessary or duplicate services. This process also helps to prevent patients from receiving ineffective or experimental treatments.
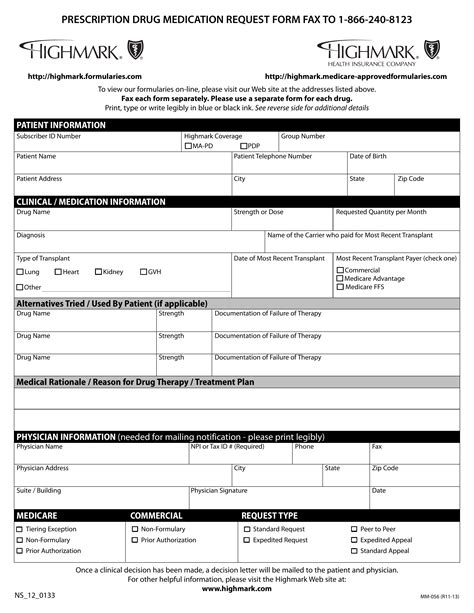
The Highmark BCBS Prior Authorization Form
The Highmark BCBS prior authorization form is a document that healthcare providers must complete to request prior authorization for a patient's treatment or procedure. The form typically requires the following information:
- Patient demographics and insurance information
- Diagnosis and treatment plan
- Procedure or medication details
- Justification for the treatment or procedure

Step-by-Step Guide to Completing the Highmark BCBS Prior Authorization Form
To ensure a smooth prior authorization process, follow these steps:
- Verify Patient Eligibility: Confirm the patient's insurance coverage and eligibility for prior authorization.
- Gather Required Information: Collect the necessary patient demographics, diagnosis, treatment plan, and procedure or medication details.
- Complete the Prior Authorization Form: Fill out the Highmark BCBS prior authorization form accurately and thoroughly.
- Submit the Form: Send the completed form to Highmark BCBS via fax, email, or online portal.
- Follow Up: Monitor the prior authorization status and follow up with Highmark BCBS if necessary.
Tips for a Successful Prior Authorization
To increase the likelihood of a successful prior authorization, follow these tips:
- Submit Complete and Accurate Information: Ensure that the prior authorization form is completed accurately and thoroughly.
- Provide Supporting Documentation: Include relevant medical records, test results, and other supporting documentation.
- Expedite Requests: Identify urgent or expedited requests to ensure timely processing.
- Communicate with Highmark BCBS: Establish open communication with Highmark BCBS to address any questions or concerns.
Common Challenges and Solutions
- Incomplete or Inaccurate Information: Ensure that the prior authorization form is completed accurately and thoroughly to avoid delays.
- Delays in Processing: Follow up with Highmark BCBS to ensure timely processing and address any issues promptly.
- Denied Requests: Review the denial reason and resubmit the request with additional information or justification.

The Benefits of Electronic Prior Authorization
Highmark BCBS offers electronic prior authorization (ePA) options, which can streamline the process and reduce administrative burdens. Benefits of ePA include:
- Increased Efficiency: Electronic submissions reduce paperwork and administrative tasks.
- Improved Accuracy: Automated systems reduce errors and improve data accuracy.
- Enhanced Patient Care: Electronic prior authorization enables faster treatment decisions and improved patient outcomes.
Conclusion and Next Steps
In conclusion, the Highmark BCBS prior authorization form is a critical document that requires accurate and thorough completion. By following the step-by-step guide and tips outlined in this article, healthcare providers can ensure a smooth prior authorization process. Patients and healthcare providers can also benefit from electronic prior authorization options, which can streamline the process and improve patient care.
We encourage you to share your experiences and feedback on the Highmark BCBS prior authorization process. Your input can help us improve our content and provide more valuable insights for our readers.
FAQ Section
What is prior authorization, and why is it required?
+Prior authorization, also known as pre-certification or pre-authorization, is a process that requires healthcare providers to obtain approval from the insurance provider before administering certain medical treatments or procedures.
How do I submit a prior authorization request to Highmark BCBS?
+You can submit a prior authorization request to Highmark BCBS via fax, email, or online portal. Ensure that the prior authorization form is completed accurately and thoroughly to avoid delays.
What are the benefits of electronic prior authorization?
+Electronic prior authorization (ePA) options can streamline the process, reduce administrative burdens, and improve patient care. Benefits include increased efficiency, improved accuracy, and enhanced patient care.