Simplifying the prior authorization process for HealthNet, or any healthcare organization, is crucial for efficient patient care and administrative management. Prior authorization, also known as pre-certification or pre-authorization, is a process used by health insurance companies to determine if a particular treatment, medication, or service is medically necessary and covered under the patient's health plan. When not managed effectively, this process can lead to delays in treatment, increased administrative burdens, and frustration for patients, healthcare providers, and payers alike. Here are five strategies to simplify the HealthNet prior authorization process, enhancing the overall healthcare experience for all parties involved.
Streamlining Communication Channels

Effective communication is the backbone of a simplified prior authorization process. One of the primary steps in streamlining communication channels is to utilize technology that enables direct, real-time interaction between healthcare providers and payers. This can include online portals, mobile applications, or integrated electronic health records (EHRs) that facilitate the exchange of patient information, treatment plans, and authorization requests.
Key Benefits:
- Reduced Administrative Burden: Automating manual processes minimizes the time spent on paperwork and phone calls.
- Enhanced Accuracy: Electronic submissions reduce errors associated with manual data entry.
- Faster Authorization Decisions: Real-time communication enables quicker review and decision-making processes.
Adopting Digital Solutions
The integration of digital solutions plays a crucial role in simplifying the prior authorization process. Digital platforms that support the electronic submission of prior authorization requests can significantly reduce processing times. These platforms often include features such as automated notifications, status updates, and secure messaging, further enhancing the efficiency of the process.
Standardizing Processes

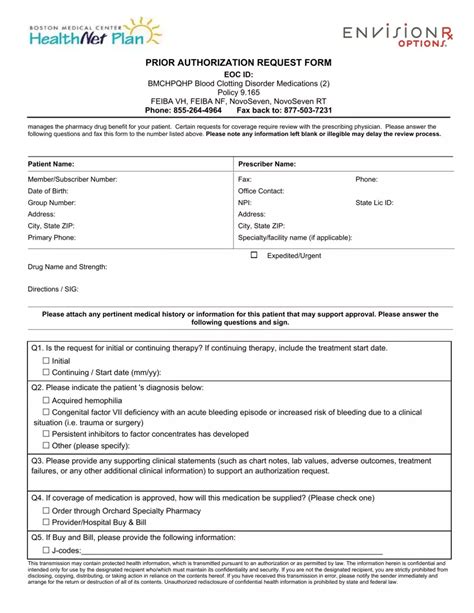
Standardizing processes involves establishing clear, consistent procedures for submitting and reviewing prior authorization requests. This can be achieved by implementing standardized forms, checklists, and criteria for determining medical necessity. Standardization helps in reducing variability and ambiguity, making the process more predictable and efficient.
Key Considerations:
- Clear Guidelines: Develop and disseminate clear guidelines on what is required for prior authorization.
- Training and Education: Provide regular training and education for staff on these standardized processes.
- Continuous Improvement: Regularly review and update processes based on feedback and performance metrics.
Empowering Patients Through Education
Educating patients about the prior authorization process is essential for managing expectations and enhancing their overall experience. This includes explaining what prior authorization is, why it is necessary, and how it affects their treatment plan. Empowered patients are more likely to be proactive in ensuring that necessary steps are taken in a timely manner.
Leveraging Data Analytics

Data analytics can provide valuable insights into the prior authorization process, helping to identify bottlenecks, trends, and areas for improvement. By analyzing data on authorization requests, approvals, denials, and processing times, healthcare providers and payers can make informed decisions to streamline the process.
Analytical Focus:
- Bottleneck Identification: Pinpoint specific stages in the process where delays occur.
- Pattern Recognition: Identify patterns in approved and denied requests to refine submission criteria.
- Process Optimization: Use data-driven insights to optimize workflows and reduce inefficiencies.
Collaborative Approach
A collaborative approach between healthcare providers, payers, and patients is fundamental in simplifying the prior authorization process. This includes open communication, mutual understanding of challenges, and a shared goal of delivering high-quality, patient-centered care.
Implementing Artificial Intelligence (AI)

Artificial intelligence (AI) and machine learning (ML) technologies can significantly enhance the efficiency and accuracy of the prior authorization process. AI can automate the review of medical records, identify required documentation, and even predict the likelihood of approval based on historical data.
AI Applications:
- Automated Review: AI can quickly review large volumes of medical records to identify necessary information.
- Predictive Analytics: AI-driven predictive models can forecast authorization outcomes.
- Personalized Communication: AI can tailor communication to individual patients based on their needs and preferences.
Future Directions
As the healthcare landscape continues to evolve, the prior authorization process must adapt to incorporate new technologies, regulatory changes, and patient needs. Future directions include further integration of AI, expansion of telehealth services, and enhanced patient engagement platforms.
What is prior authorization in healthcare?
+Prior authorization, also known as pre-certification or pre-authorization, is a process used by health insurance companies to determine if a particular treatment, medication, or service is medically necessary and covered under the patient's health plan.
How can technology simplify the prior authorization process?
+Technology can simplify the prior authorization process by enabling electronic submissions, automating manual processes, enhancing communication, and providing real-time updates.
What role does patient education play in simplifying prior authorization?
+Patient education empowers patients to be proactive in their care, understand the prior authorization process, and manage expectations, thereby enhancing their overall experience.
In conclusion, simplifying the HealthNet prior authorization process is multifaceted, involving the integration of technology, standardization of processes, empowerment through education, leveraging of data analytics, and a collaborative approach. By implementing these strategies, healthcare providers, payers, and patients can work together to ensure that necessary treatments are accessed in a timely and efficient manner, ultimately enhancing the quality of care and the patient experience.