Healthfirst is a not-for-profit health insurance company that provides coverage to individuals and families in New York City and Long Island. One of the key aspects of managing healthcare costs is the prior authorization process, which requires healthcare providers to obtain approval from Healthfirst before administering certain treatments or services. In this article, we will provide a step-by-step guide on how to complete the Healthfirst prior authorization form.
Understanding the Importance of Prior Authorization
Prior authorization is a critical process in healthcare that ensures patients receive necessary and cost-effective treatments. It also helps prevent unnecessary costs and ensures that patients receive the right care at the right time. Healthfirst requires prior authorization for certain services, including prescription medications, medical procedures, and specialized treatments. By completing the prior authorization form, healthcare providers can ensure that their patients receive the necessary approvals for treatment.

Step 1: Determine If Prior Authorization Is Required
Before completing the prior authorization form, healthcare providers must determine if prior authorization is required for the specific service or treatment. Healthfirst provides a list of services that require prior authorization on their website. Providers can also contact Healthfirst's customer service department to confirm if prior authorization is required.
Services That Require Prior Authorization
Some examples of services that require prior authorization from Healthfirst include:
- Prescription medications for certain conditions, such as cancer or multiple sclerosis
- Medical procedures, such as MRI or CT scans
- Specialized treatments, such as dialysis or chemotherapy
- Durable medical equipment, such as wheelchairs or oxygen tanks
Step 2: Gather Required Information
Once it is determined that prior authorization is required, healthcare providers must gather the necessary information to complete the form. This includes:
- Patient demographics, such as name, date of birth, and Healthfirst ID number
- Provider information, such as name, NPI number, and office address
- Service or treatment details, such as procedure code, date of service, and diagnosis code
- Supporting documentation, such as medical records or test results

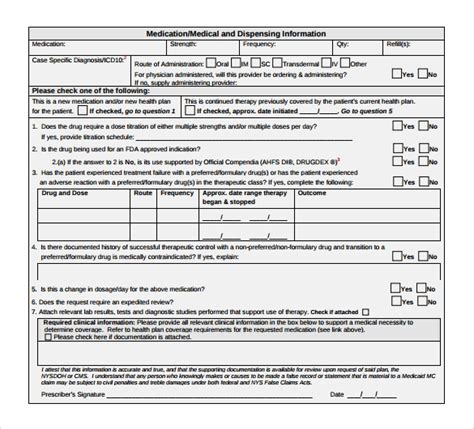
Step 3: Complete the Prior Authorization Form
The Healthfirst prior authorization form can be completed online or by fax. Providers can access the online form through Healthfirst's provider portal. The form requires providers to enter the necessary information, including patient demographics, provider information, and service or treatment details.
Online Form Completion
To complete the online form, providers must:
- Log in to Healthfirst's provider portal
- Select the "Prior Authorization" option
- Enter the required information, including patient demographics and service details
- Upload supporting documentation, such as medical records or test results
- Submit the form for review
Step 4: Submit the Prior Authorization Form
Once the form is complete, providers must submit it to Healthfirst for review. This can be done online or by fax. Providers should ensure that all required information is included and that the form is complete to avoid delays in the review process.

Step 5: Follow Up on the Prior Authorization Request
After submitting the prior authorization form, providers should follow up on the status of the request. Healthfirst provides a timeline for review and approval, which can be found on their website. Providers can also contact Healthfirst's customer service department to check on the status of the request.
Timeline for Review and Approval
Healthfirst's timeline for review and approval is as follows:
- Standard review: 3-5 business days
- Expedited review: 1-2 business days
- Urgent review: same day or next business day
Conclusion
Completing the Healthfirst prior authorization form is a critical step in ensuring that patients receive necessary and cost-effective treatments. By following these steps, healthcare providers can ensure that their patients receive the necessary approvals for treatment. We encourage providers to comment below with any questions or concerns about the prior authorization process.
What is prior authorization?
+Prior authorization is a process that requires healthcare providers to obtain approval from Healthfirst before administering certain treatments or services.
What services require prior authorization?
+Services that require prior authorization from Healthfirst include prescription medications, medical procedures, specialized treatments, and durable medical equipment.
How long does the prior authorization review process take?
+Healthfirst's timeline for review and approval is as follows: standard review: 3-5 business days, expedited review: 1-2 business days, urgent review: same day or next business day.