In today's complex healthcare landscape, Prior Authorization (PA) plays a crucial role in ensuring that patients receive the necessary treatments while controlling costs. For healthcare providers, submitting a Prior Authorization request form can be a daunting task, especially when dealing with FirstCare, a popular health insurance provider. To simplify the process and increase the chances of approval, we've compiled 5 valuable tips for submitting a FirstCare Prior Authorization request form.
Understanding the Importance of Prior Authorization
Prior Authorization is a process where healthcare providers must obtain approval from the insurance company before administering certain treatments, medications, or procedures. This step is essential in preventing unnecessary costs and ensuring that patients receive the most effective and evidence-based care. For healthcare providers, navigating the Prior Authorization process can be time-consuming and frustrating, but with the right approach, it can also be a streamlined and efficient process.
Tip 1: Verify Patient Eligibility and Benefits
Before submitting a Prior Authorization request form, it's essential to verify the patient's eligibility and benefits with FirstCare. This step ensures that the patient is covered for the specific treatment or service being requested. Healthcare providers can use FirstCare's online portal or contact their customer service department to verify patient information. By doing so, providers can avoid unnecessary delays and rework.

Tip 2: Gather Required Documentation
To increase the chances of approval, healthcare providers must gather all required documentation, including:
- Patient demographics and medical history
- Treatment plans and medical records
- Relevant lab results and test reports
- Prescriptions and medication lists
By providing comprehensive documentation, providers can demonstrate the medical necessity of the requested treatment and reduce the likelihood of delays or denials.
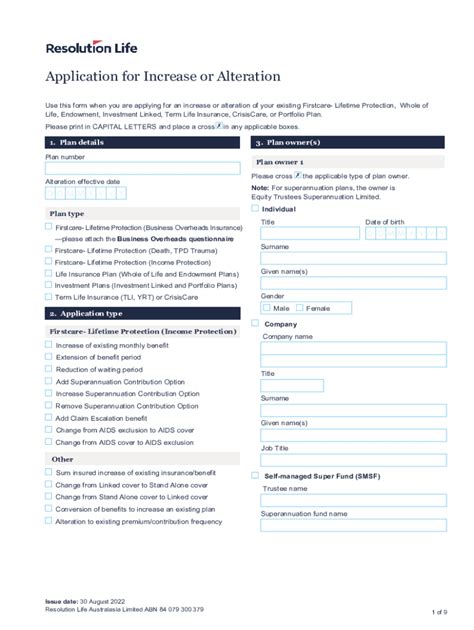
Tip 3: Complete the Request Form Accurately
The Prior Authorization request form is a critical component of the submission process. Healthcare providers must complete the form accurately and thoroughly, ensuring that all required fields are populated and supporting documentation is attached. FirstCare's online portal provides a user-friendly interface for submitting Prior Authorization requests, but providers can also use fax or mail if preferred.

Tip 4: Submit the Request in a Timely Manner
Timely submission of the Prior Authorization request is crucial in ensuring that patients receive the necessary treatments without delays. Healthcare providers should submit the request form at least 7-10 business days before the scheduled treatment or service. This allows FirstCare sufficient time to review the request and render a decision.
Tip 5: Follow Up and Escalate as Necessary
After submitting the Prior Authorization request form, healthcare providers should follow up with FirstCare to ensure that the request is being processed. If the request is denied or delayed, providers can escalate the issue to FirstCare's appeals department. By being proactive and persistent, providers can advocate for their patients and increase the chances of approval.

What's Next?
By following these 5 tips, healthcare providers can streamline the Prior Authorization process and increase the chances of approval for their patients. Remember to:
- Verify patient eligibility and benefits
- Gather required documentation
- Complete the request form accurately
- Submit the request in a timely manner
- Follow up and escalate as necessary
By taking a proactive and informed approach to the Prior Authorization process, healthcare providers can improve patient outcomes and reduce administrative burdens.
What is Prior Authorization, and why is it necessary?
+Prior Authorization is a process where healthcare providers must obtain approval from the insurance company before administering certain treatments, medications, or procedures. This step is essential in preventing unnecessary costs and ensuring that patients receive the most effective and evidence-based care.
How long does the Prior Authorization process typically take?
+The Prior Authorization process typically takes 7-10 business days, but this may vary depending on the complexity of the request and the efficiency of the provider's submission process.
What happens if the Prior Authorization request is denied?
+If the Prior Authorization request is denied, healthcare providers can appeal the decision to FirstCare's appeals department. Providers should provide additional documentation or information to support the request and advocate for their patients.