As a healthcare provider, managing prior authorizations can be a complex and time-consuming process. Fidelis is a leading healthcare management company that offers a range of services, including prior authorization. In this article, we will guide you through the 5 easy steps to complete a Fidelis prior authorization form.
The importance of prior authorization cannot be overstated. It ensures that patients receive the necessary medical treatment while also controlling healthcare costs. However, the process can be lengthy and requires accurate documentation. With Fidelis, you can streamline your prior authorization process, reducing administrative burdens and improving patient outcomes.
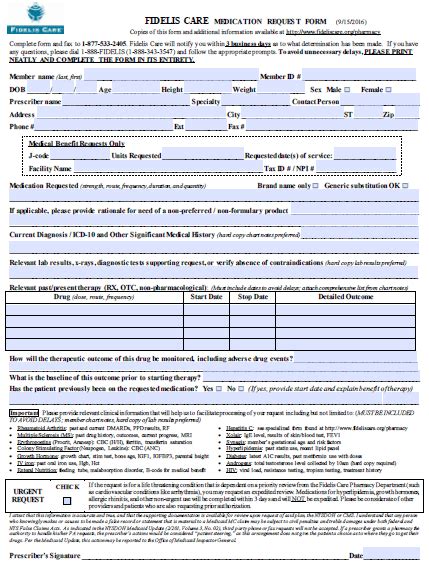
Understanding the Fidelis Prior Authorization Form

The Fidelis prior authorization form is a crucial document that requires accurate and complete information. It's essential to understand the form's layout and the information required to avoid delays or rejections. The form typically includes sections for patient demographics, medical history, treatment details, and provider information.
What Information is Required?
To complete the Fidelis prior authorization form, you will need to provide the following information:
- Patient demographics, including name, date of birth, and contact information
- Medical history, including diagnosis, symptoms, and treatment history
- Treatment details, including medication, dosage, and frequency
- Provider information, including name, license number, and contact information
Step 1: Gather Required Documents and Information

Before starting the prior authorization process, ensure you have all the necessary documents and information. This includes:
- Patient's medical records, including test results and treatment plans
- Prescription medication list
- Insurance cards and identification documents
- Provider information, including license numbers and contact details
Why is this Step Important?
Gathering all the required documents and information upfront saves time and reduces the likelihood of errors or delays. It's essential to ensure that all information is accurate and up-to-date to avoid rejections or additional requests for information.
Step 2: Complete the Fidelis Prior Authorization Form

Using the gathered information, complete the Fidelis prior authorization form. Ensure that all sections are filled out accurately and thoroughly. If you're unsure about any information, consult with the patient or their medical records.
Tips for Completing the Form
- Use black ink and print clearly
- Avoid abbreviations or acronyms
- Include all relevant medical information
- Double-check for errors or omissions
Step 3: Submit the Fidelis Prior Authorization Form

Once the form is complete, submit it to Fidelis via fax, email, or online portal. Ensure that you follow the submission guidelines carefully to avoid delays or rejections.
What Happens After Submission?
After submitting the prior authorization form, Fidelis will review the information and make a determination. If additional information is required, you will be notified. Once approved, the patient's treatment can proceed.
Step 4: Follow-up on the Prior Authorization Status

It's essential to follow up on the prior authorization status to ensure that the patient's treatment is not delayed. You can check the status online or contact Fidelis directly.
Why is Follow-up Important?
Follow-up ensures that any issues or delays are addressed promptly, reducing the risk of treatment delays or denials.
Step 5: Receive Prior Authorization Approval

Once the prior authorization is approved, you will receive notification from Fidelis. The patient's treatment can then proceed, and you can focus on providing the best possible care.
What's Next?
After receiving prior authorization approval, ensure that the patient's treatment plan is implemented, and their progress is monitored.
We hope this article has provided you with a clear understanding of the 5 easy steps to complete a Fidelis prior authorization form. By following these steps, you can streamline your prior authorization process, reducing administrative burdens and improving patient outcomes.
We invite you to share your experiences with Fidelis prior authorization forms in the comments below. Your feedback can help us improve our content and provide better support for healthcare providers.
Don't forget to share this article with your colleagues and friends who may benefit from this information.
What is the purpose of a prior authorization form?
+The purpose of a prior authorization form is to ensure that patients receive necessary medical treatment while controlling healthcare costs.
What information is required on the Fidelis prior authorization form?
+The form requires patient demographics, medical history, treatment details, and provider information.
How do I submit the Fidelis prior authorization form?
+You can submit the form via fax, email, or online portal, following the submission guidelines carefully.