Simplifying Federal BCBS Prior Authorization: Understanding the Process

Federal BCBS prior authorization can be a complex and time-consuming process for healthcare providers and patients alike. The process involves obtaining approval from Blue Cross Blue Shield (BCBS) before providing certain medical services or treatments. In this article, we will break down the process into 5 easy steps, making it simpler for you to understand and navigate.
Why is Prior Authorization Necessary?
Prior authorization is a crucial step in ensuring that patients receive necessary medical care while also managing healthcare costs. By reviewing and approving medical services before they are provided, BCBS can:
- Ensure that patients receive evidence-based care
- Reduce unnecessary medical procedures and costs
- Improve patient outcomes and safety
How Does Prior Authorization Work?
Prior authorization involves a series of steps that healthcare providers and patients must follow. Here are the 5 easy steps to simplify the process:
Step 1: Verify Patient Eligibility

Before initiating the prior authorization process, healthcare providers must verify the patient's eligibility for BCBS coverage. This involves checking the patient's membership status, benefits, and any applicable exclusions or limitations.
What Information is Needed?
To verify patient eligibility, healthcare providers need to gather the following information:
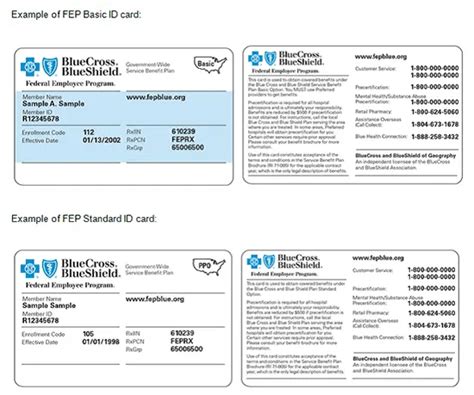
- Patient's name and date of birth
- BCBS membership ID number
- Policy effective date and expiration date (if applicable)
Step 2: Determine Prior Authorization Requirements

Once patient eligibility is verified, healthcare providers must determine if prior authorization is required for the specific medical service or treatment. This involves checking the BCBS prior authorization list, which outlines the services and treatments that require approval.
What Services Require Prior Authorization?
BCBS typically requires prior authorization for services such as:
- Non-emergency hospital admissions
- Outpatient surgeries
- Advanced imaging services (e.g., MRI, CT scans)
- Specialty medications
Step 3: Gather Required Documentation

After determining that prior authorization is required, healthcare providers must gather the necessary documentation to support the request. This may include:
- Medical records and test results
- Treatment plans and diagnoses
- Medication lists and dosages
What Documentation is Needed?
The specific documentation required may vary depending on the medical service or treatment. However, healthcare providers should always include:
- A clear and concise description of the medical service or treatment
- Relevant medical records and test results
- A statement explaining why prior authorization is necessary
Step 4: Submit the Prior Authorization Request

Once the required documentation is gathered, healthcare providers can submit the prior authorization request to BCBS. This can be done online, by phone, or by mail.
How to Submit the Request?
Healthcare providers can submit the prior authorization request through:
- BCBS online portal
- Phone (by calling the BCBS customer service number)
- Mail (by sending the request to the BCBS mailing address)
Step 5: Receive Prior Authorization Approval or Denial

After submitting the prior authorization request, healthcare providers will receive a response from BCBS indicating whether the request is approved or denied.
What Happens Next?
If the request is approved, healthcare providers can proceed with providing the medical service or treatment. If the request is denied, healthcare providers can appeal the decision or explore alternative treatment options.
Conclusion: Simplifying Federal BCBS Prior Authorization
Federal BCBS prior authorization can be a complex process, but by following these 5 easy steps, healthcare providers and patients can navigate the process with ease. By verifying patient eligibility, determining prior authorization requirements, gathering required documentation, submitting the request, and receiving approval or denial, healthcare providers can ensure that patients receive necessary medical care while also managing healthcare costs.
We encourage you to share your experiences with Federal BCBS prior authorization in the comments below. If you have any questions or need further clarification on the process, please don't hesitate to ask.
What is prior authorization?
+Prior authorization is a process where healthcare providers must obtain approval from Blue Cross Blue Shield (BCBS) before providing certain medical services or treatments.
Why is prior authorization necessary?
+Prior authorization is necessary to ensure that patients receive evidence-based care, reduce unnecessary medical procedures and costs, and improve patient outcomes and safety.
How long does the prior authorization process take?
+The prior authorization process typically takes 1-3 business days, but may vary depending on the complexity of the request and the availability of necessary documentation.