Prior authorization is a crucial step in the healthcare process, ensuring that patients receive the right treatment while controlling costs. For pharmacies, managing prior authorization requests can be a daunting task, especially when dealing with multiple payers and complex regulations. That's where Envolve Pharmacy Solutions comes in - a leading provider of pharmacy benefit management services. In this article, we'll explore the Envolve Pharmacy Solutions prior authorization form and how it can be made easy for pharmacies and patients alike.
What is Prior Authorization?
Prior authorization is a process where healthcare providers or pharmacies obtain approval from payers (insurance companies or government programs) before prescribing or dispensing certain medications. This ensures that the medication is medically necessary and cost-effective. Prior authorization helps control healthcare costs, prevents unnecessary medication use, and ensures patient safety.

Challenges with Prior Authorization
While prior authorization is essential, the process can be cumbersome, leading to delays and frustration for pharmacies, patients, and healthcare providers. Common challenges include:
- Complexity: Prior authorization forms and processes can be convoluted, leading to errors and misinterpretation.
- Time-consuming: Gathering required information and submitting forms can be a time-consuming process, delaying patient care.
- Communication breakdowns: Poor communication between pharmacies, payers, and healthcare providers can lead to miscommunication and delayed approvals.
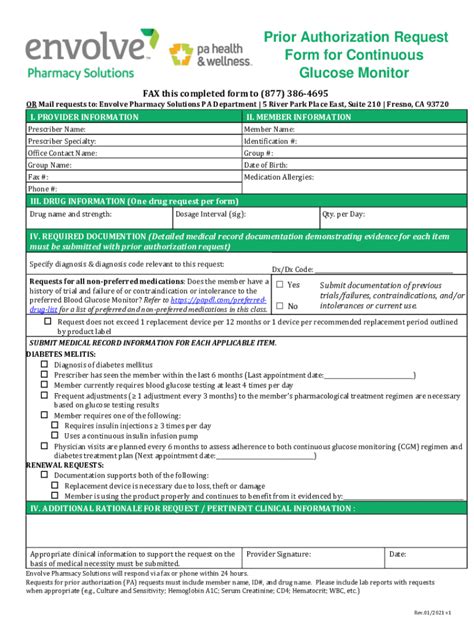
Envolve Pharmacy Solutions Prior Authorization Form
Envolve Pharmacy Solutions offers a streamlined prior authorization process, designed to simplify the workflow for pharmacies and healthcare providers. Their prior authorization form is electronic, reducing paperwork and increasing efficiency. The form is also easy to navigate, with clear instructions and required fields.

Benefits of the Envolve Pharmacy Solutions Prior Authorization Form
The Envolve Pharmacy Solutions prior authorization form offers several benefits, including:
- Streamlined workflow: Electronic forms reduce paperwork and increase processing speed.
- Improved accuracy: Required fields and clear instructions minimize errors.
- Enhanced communication: Real-time notifications and online tracking ensure that all parties are informed.
- Reduced delays: Faster processing times mean quicker approvals and improved patient care.
How to Make the Prior Authorization Process Easier
While the Envolve Pharmacy Solutions prior authorization form is designed to be user-friendly, there are additional steps pharmacies and healthcare providers can take to make the process even easier:
- Familiarize yourself with the form: Take time to understand the required fields and instructions.
- Gather necessary information: Ensure that all necessary patient and medication information is readily available.
- Use online resources: Take advantage of online tutorials and support resources to help navigate the form.
- Stay organized: Keep track of submitted forms and follow up on pending approvals.

Best Practices for Prior Authorization
To ensure a smooth prior authorization process, follow these best practices:
- Verify patient eligibility: Confirm patient coverage and eligibility before submitting the form.
- Use current medication lists: Ensure that the patient's medication list is up-to-date and accurate.
- Provide clear documentation: Include all required documentation, such as medical records and test results.
- Follow up: Regularly check on the status of pending approvals and follow up with payers as needed.
Conclusion: Simplifying Prior Authorization with Envolve Pharmacy Solutions
Prior authorization is an essential step in the healthcare process, but it can be a complex and time-consuming process. Envolve Pharmacy Solutions offers a streamlined prior authorization form that simplifies the workflow for pharmacies and healthcare providers. By understanding the benefits of the form and following best practices, pharmacies and healthcare providers can make the prior authorization process easier, reducing delays and improving patient care.

We invite you to share your thoughts on the prior authorization process and how you've simplified it in your pharmacy or healthcare practice. Your insights can help others navigate this complex process and improve patient care.
What is prior authorization?
+Prior authorization is a process where healthcare providers or pharmacies obtain approval from payers (insurance companies or government programs) before prescribing or dispensing certain medications.
What are the benefits of the Envolve Pharmacy Solutions prior authorization form?
+The Envolve Pharmacy Solutions prior authorization form offers several benefits, including a streamlined workflow, improved accuracy, enhanced communication, and reduced delays.
How can I simplify the prior authorization process?
+To simplify the prior authorization process, familiarize yourself with the form, gather necessary information, use online resources, and stay organized. Additionally, follow best practices such as verifying patient eligibility, using current medication lists, providing clear documentation, and following up on pending approvals.