Navigating the complex world of healthcare can be daunting, especially when it comes to accessing essential medications. For patients relying on Dupixent, a crucial medication for treating moderate-to-severe atopic dermatitis, asthma, and other conditions, understanding the prior authorization process is vital. CVS Caremark, a leading pharmacy benefit management company, plays a significant role in managing this process. In this comprehensive guide, we will delve into the CVS Caremark Dupixent prior authorization form, its importance, and how to navigate the process efficiently.
Understanding Prior Authorization

Prior authorization is a process used by health insurance companies and pharmacy benefit managers to determine whether a prescribed medication is medically necessary and meets specific criteria before approving coverage. This process aims to ensure that patients receive the most effective and cost-efficient treatment options. For medications like Dupixent, which can be costly and have specific usage guidelines, prior authorization is often required.
Why is Prior Authorization Important?
Prior authorization is crucial for several reasons:
- Ensures Appropriate Use: It guarantees that medications are prescribed and used appropriately, adhering to established clinical guidelines.
- Cost Management: By evaluating the medical necessity of a medication, prior authorization helps manage healthcare costs and prevent unnecessary expenses.
- Patient Safety: The process ensures that patients receive medications that are safe and effective for their specific condition, reducing the risk of adverse reactions or interactions.
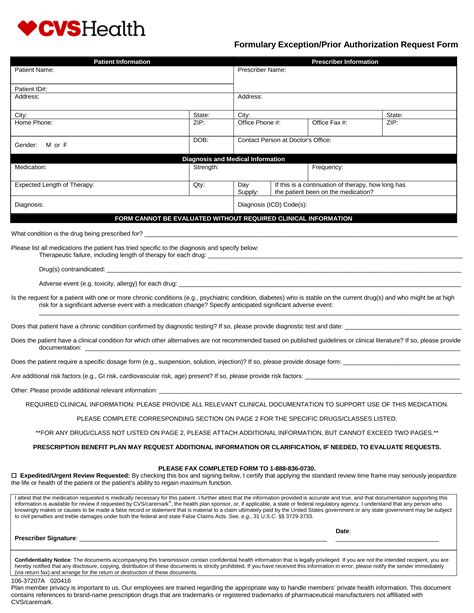
The CVS Caremark Dupixent Prior Authorization Form

The CVS Caremark Dupixent prior authorization form is a document that healthcare providers must complete and submit to CVS Caremark for review. This form requires detailed patient information, medical history, and specifics about the prescribed medication, including dosage and duration of treatment.
Key Information Required on the Form:
- Patient Demographics: Full name, date of birth, and contact information.
- Medication Details: Name, dosage, frequency, and duration of Dupixent treatment.
- Medical History: Relevant medical conditions, allergies, and previous treatments.
- Clinical Justification: A clear explanation of why Dupixent is medically necessary for the patient's condition.
How to Complete and Submit the Form
Completing the CVS Caremark Dupixent prior authorization form accurately and thoroughly is crucial for a successful review process. Here are steps to follow:
- Download or Obtain the Form: Access the form through the CVS Caremark website or request it from your healthcare provider.
- Gather Required Information: Ensure you have all necessary patient and medication details before starting the form.
- Complete the Form: Fill out the form accurately and completely. Incomplete forms may delay the review process.
- Submit the Form: Fax or mail the completed form to CVS Caremark, following the instructions provided.
Tips for a Smooth Prior Authorization Process

To ensure a smooth and efficient prior authorization process for Dupixent, consider the following tips:
- Plan Ahead: Initiate the prior authorization process well in advance of the patient's need for the medication.
- Complete Accurate Submissions: Ensure all required information is accurate and complete to avoid delays.
- Follow Up: If necessary, follow up with CVS Caremark to check the status of the prior authorization request.
Common Challenges and Solutions
While the prior authorization process is designed to ensure appropriate medication use, it can sometimes present challenges. Here are common issues and potential solutions:
- Delays in Approval: Expedite the process by ensuring complete and accurate submissions and following up with CVS Caremark.
- Denials: If a request is denied, review the reason and resubmit with additional information or appeal the decision if necessary.
Conclusion and Next Steps

Navigating the CVS Caremark Dupixent prior authorization process requires patience, attention to detail, and understanding of the requirements. By following the guidelines outlined in this comprehensive guide, healthcare providers and patients can ensure a smoother experience.
Take Action:
- Share this guide with colleagues and patients to enhance understanding of the prior authorization process.
- Visit the CVS Caremark website for the latest information on prior authorization forms and processes.
- Engage in discussions below to share experiences or ask questions about the CVS Caremark Dupixent prior authorization form.
FAQ Section
What is the purpose of the CVS Caremark Dupixent prior authorization form?
+The form is used to determine whether Dupixent is medically necessary for a patient's condition, ensuring appropriate use and cost management.
How long does the prior authorization process typically take?
+The processing time can vary, but it generally takes a few days to a week. Planning ahead and submitting complete information can help expedite the process.
What if my prior authorization request for Dupixent is denied?
+If denied, review the reason for denial and consider resubmitting with additional information or appealing the decision if necessary.